Final ID: MDP552
Cardiovascular Prognosis in Patients with Diabetes Mellitus Mediated by the Functional Post-revascularization Level
Abstract Body (Do not enter title and authors here): Background and Aims: Functional complete revascularization (FCR) subsequent to percutaneous coronary intervention (PCI), as assessed by the residual functional SYNTAX score (rFSS), has been correlated with enhanced prognostic outcomes. This study sought to comprehensively apprehend the adverse cardiovascular prognosis within diabetic cohorts, determining what extent the association of diabetes with clinical outcomes is explained by functional revascularization.
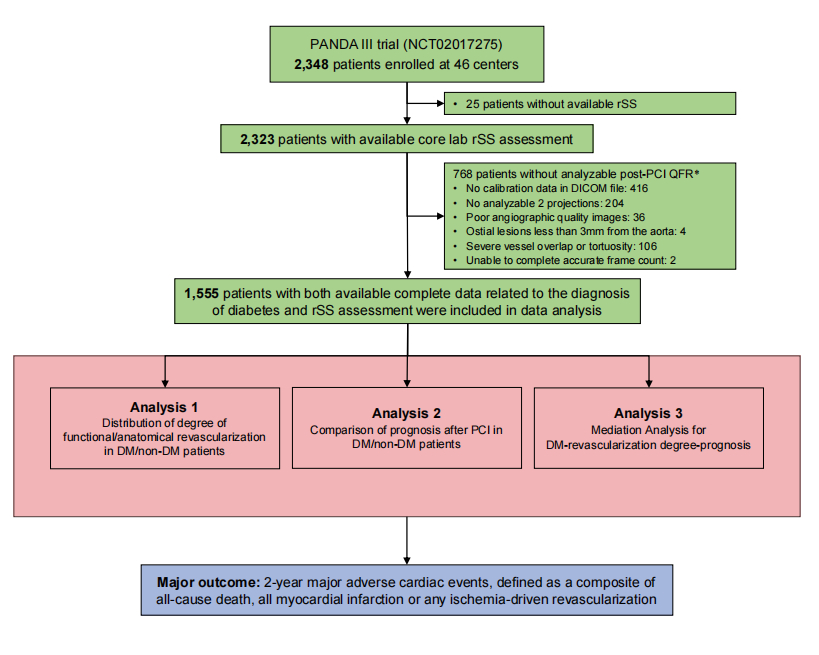
Methods: A total of 1,555 patients with available post-PCI quantitative flow ratio (QFR) were included, whose data were collected from PANDA III trial (Figure 1). FCR was defined as rFSS = 0, while anatomic complete revascularization (ACR) was defined as residual SYNTAX score (rSS) = 0. Firstly, we determined the ACR and FCR among DM and non-DM cohorts. Second, multiple cox regression was used to screen for potential mediating variables. Finally, we used structural equation modeling to analysis whether FCR explained the relationship between DM and the risk of 2-year rates of major adverse cardiac events (MACE).
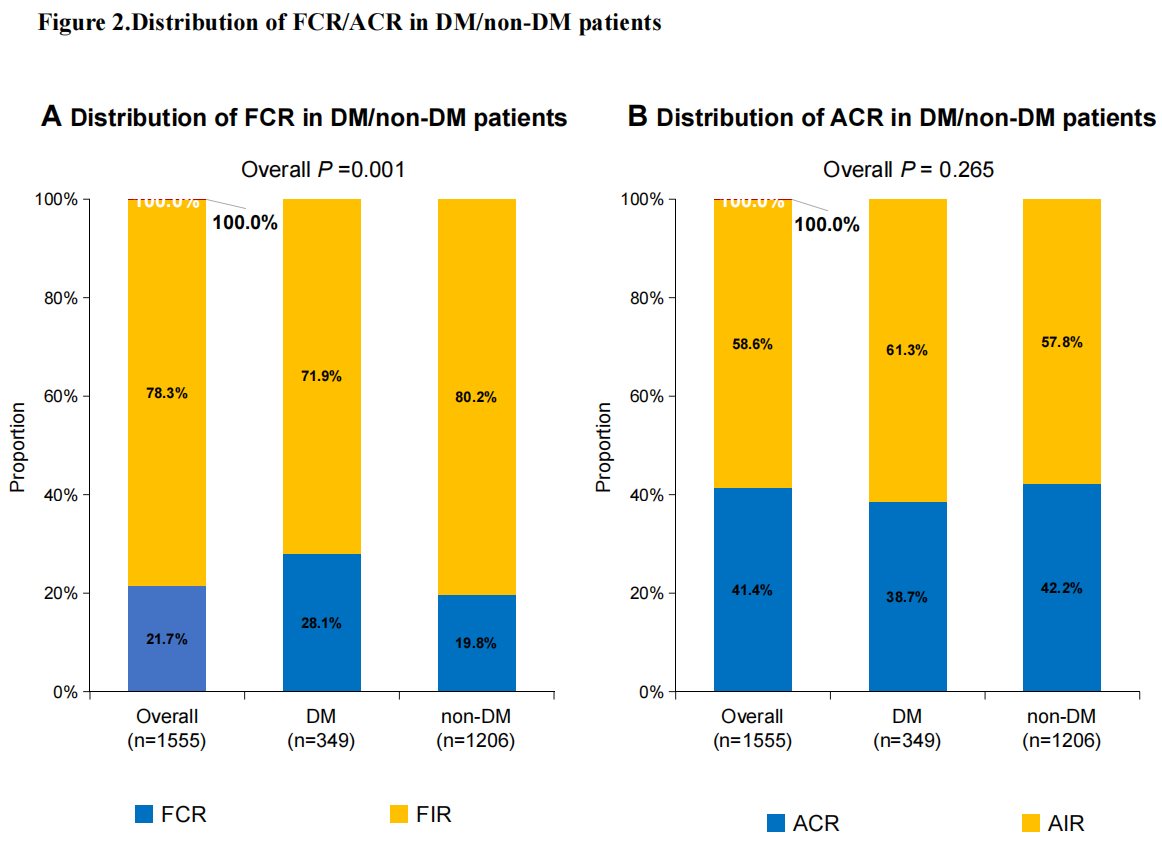
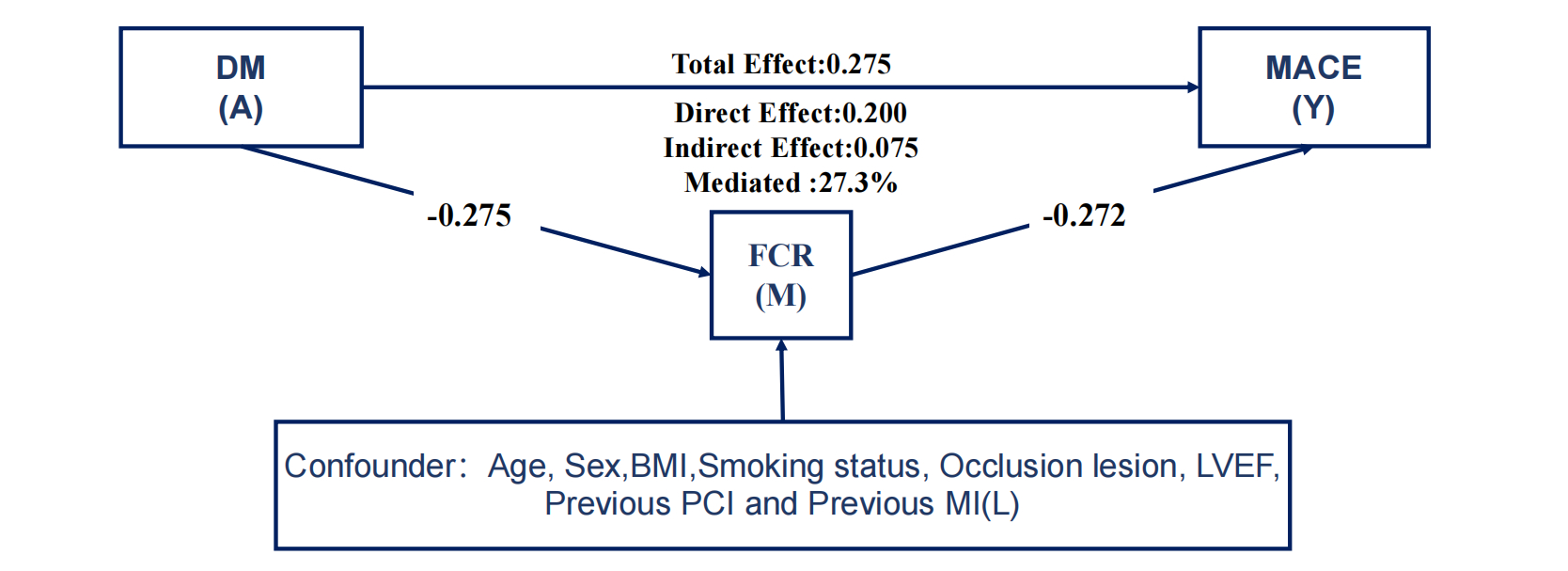
Results: Patients with DM had a significant lower percentage of FCR (71.9% vs 80.2%, P<0.001), however ACR was not (38.68 vs 42.21, P=0.265, Figure 2). Multiple cox regression revealed that DM was associated with MACE (P=0.007), but not after adding FCR to the model (P=0.05), suggesting a mediation effect. Structural equation modeling analysis revealed a significant indirect effect of DM on MACE through FCR (P=0.006, Mediated (%) =27.3,Figure 3), suggesting a partial mediation effect.
Conclusion: The degree of functional revascularization emerges as a central mechanism pivotal in elucidating the association between DM and the risk of MACE.
Methods: A total of 1,555 patients with available post-PCI quantitative flow ratio (QFR) were included, whose data were collected from PANDA III trial (Figure 1). FCR was defined as rFSS = 0, while anatomic complete revascularization (ACR) was defined as residual SYNTAX score (rSS) = 0. Firstly, we determined the ACR and FCR among DM and non-DM cohorts. Second, multiple cox regression was used to screen for potential mediating variables. Finally, we used structural equation modeling to analysis whether FCR explained the relationship between DM and the risk of 2-year rates of major adverse cardiac events (MACE).
Results: Patients with DM had a significant lower percentage of FCR (71.9% vs 80.2%, P<0.001), however ACR was not (38.68 vs 42.21, P=0.265, Figure 2). Multiple cox regression revealed that DM was associated with MACE (P=0.007), but not after adding FCR to the model (P=0.05), suggesting a mediation effect. Structural equation modeling analysis revealed a significant indirect effect of DM on MACE through FCR (P=0.006, Mediated (%) =27.3,Figure 3), suggesting a partial mediation effect.
Conclusion: The degree of functional revascularization emerges as a central mechanism pivotal in elucidating the association between DM and the risk of MACE.
More abstracts on this topic:
Artificial Intelligence ECG-Extracted Features Predict Microvascular Obstruction in ST-segment Elevation Myocardial Infarction
Traverse Jay, Meyers Pendell, Sharkey Scott, Schwager Sarah, Stanberry Larissa, Herman Robert
Aspirin for Primary Prevention of Cardiovascular Events in Patients with Diabetes Mellitus: An Updated Systematic Review, Meta-Analysis & Trial Sequential Analysis of Randomized Controlled Trials post-ASCEND TrialPuthia Valappil Omer Mohammed, John M Rose, Mallikarjun Samanth, D Souza Leroy, Rongala Sai Anurag, Chakraborty Diya, Balarishnan Rojith, Kutty Shelby