Final ID: Su3093
Aspirin Use among Women at High-Risk for Pre-eclampsia in the United States
Abstract Body (Do not enter title and authors here): Background
Pre-eclampsia is a major cause of maternal and neonatal morbidity and mortality and impacts 5-7% of pregnancies. Randomized trials have shown that aspirin reduces the risk of pre-eclampsia by 10-20%. In 2018, ACOG recommended the use of aspirin in high-risk women and “consideration” in those with moderate risk factors, which would newly include African American race. We sought to determine the proportion of women at risk for pre-eclampsia in the US receiving aspirin and how new guidelines impacted use.
Methods
We used survey data from the National Ambulatory Medical Care Survey (NAMCS), a nationally representative survey conducted by the CDC of ambulatory health visits. We assessed visits of pregnant women from 2014-6 and 2018-9 and examined aspirin use according to pre-eclampsia risk status. High-risk includes those with hypertension, diabetes, or chronic kidney disease; medium-risk includes those with >=2 of the following: Black race, low socioeconomic status (identified by Medicaid enrollment), obesity, and age >=35. To determine if aspirin use was well-captured, we tested validity using coronary heart disease.
Results
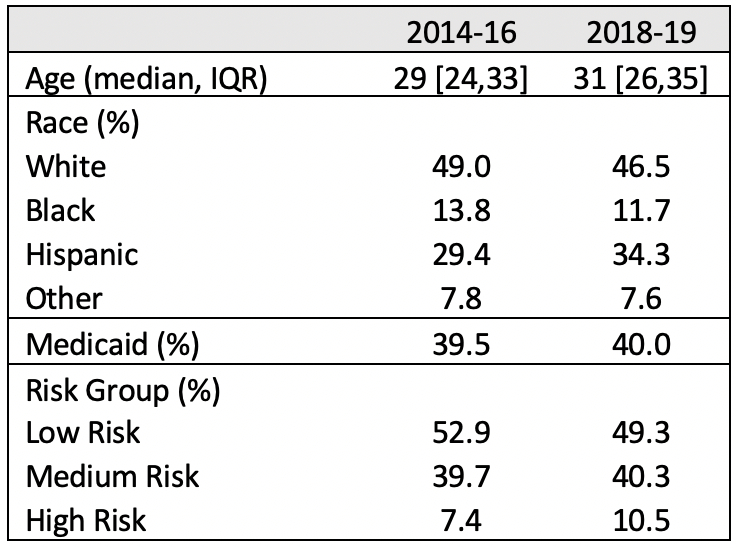
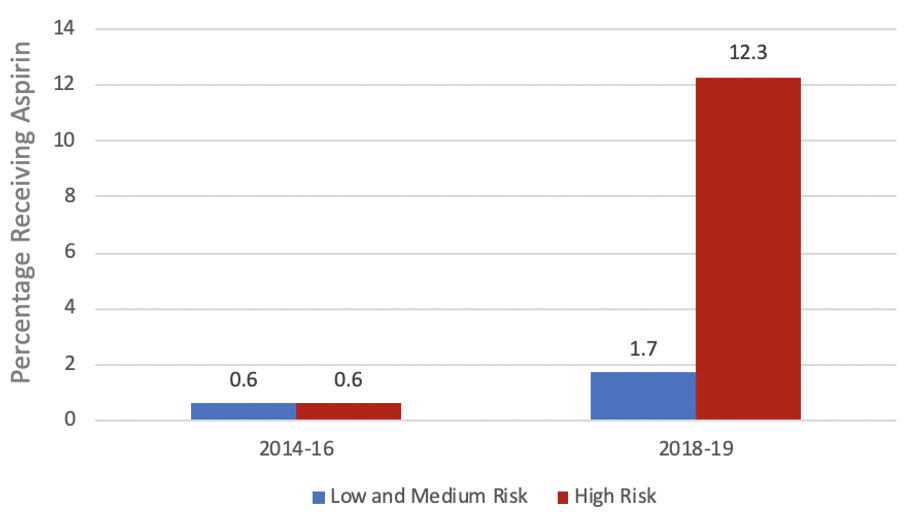
We identified 3,362 visits among pregnant women 2014-9, of which 8.3% occurred with high-risk women (Table 1). Aspirin use increased modestly at visits among low- and medium-risk women after guideline publication, to 1.7% (95% CI 0.5-3.9%) of visits in 2018-9. In contrast, aspirin use increased substantially at visits with high-risk women, though still remained low at 12.3% (95% CI 3.9-27%).
Conclusions
Aspirin is an inexpensive and accessible intervention to reduce pre-eclampsia, a driver of adverse pregnancy outcomes and observed racial disparities. Aspirin use in moderate-risk women had minimal change over the time period, suggesting little immediate impact of the 2018 guidelines. Use in high-risk women increased significantly, but still remains low. Systematic efforts to ensure widespread and equitable use of this therapy are needed.
Pre-eclampsia is a major cause of maternal and neonatal morbidity and mortality and impacts 5-7% of pregnancies. Randomized trials have shown that aspirin reduces the risk of pre-eclampsia by 10-20%. In 2018, ACOG recommended the use of aspirin in high-risk women and “consideration” in those with moderate risk factors, which would newly include African American race. We sought to determine the proportion of women at risk for pre-eclampsia in the US receiving aspirin and how new guidelines impacted use.
Methods
We used survey data from the National Ambulatory Medical Care Survey (NAMCS), a nationally representative survey conducted by the CDC of ambulatory health visits. We assessed visits of pregnant women from 2014-6 and 2018-9 and examined aspirin use according to pre-eclampsia risk status. High-risk includes those with hypertension, diabetes, or chronic kidney disease; medium-risk includes those with >=2 of the following: Black race, low socioeconomic status (identified by Medicaid enrollment), obesity, and age >=35. To determine if aspirin use was well-captured, we tested validity using coronary heart disease.
Results
We identified 3,362 visits among pregnant women 2014-9, of which 8.3% occurred with high-risk women (Table 1). Aspirin use increased modestly at visits among low- and medium-risk women after guideline publication, to 1.7% (95% CI 0.5-3.9%) of visits in 2018-9. In contrast, aspirin use increased substantially at visits with high-risk women, though still remained low at 12.3% (95% CI 3.9-27%).
Conclusions
Aspirin is an inexpensive and accessible intervention to reduce pre-eclampsia, a driver of adverse pregnancy outcomes and observed racial disparities. Aspirin use in moderate-risk women had minimal change over the time period, suggesting little immediate impact of the 2018 guidelines. Use in high-risk women increased significantly, but still remains low. Systematic efforts to ensure widespread and equitable use of this therapy are needed.
More abstracts on this topic:
Aspirin-Nanoparticle for Dual Therapies: Targeted Anti-Inflammatory and Prolonged Anti-Platelet Effects for Atherosclerosis
Chung Seyong, Yu Seung Eun, Jueun Kim
Adoptive transfer of placental CD4+ T Cells from preeclamptic patients with a history of COVID-19 causes hypertension and cognitive dysfunction postpartum in a pregnant rat model of preeclampsiaDeer Evangeline, Simmons Kimberly, Herrock Owen, Campbell Nathan, Roman Richard, Zheng Baoying, Morris Rachael, Lamarca Babbette