Final ID: Su4026
Prevalence and Outcomes of Percutaneous Coronary Intervention in Patients With and Without Bipolar Disorder: A National Inpatient Sample Analysis
Abstract Body (Do not enter title and authors here): Background: Severe mental disorders (SMIs) such as bipolar disorder are associated with a reduced life expectancy of up to two decades, with cardiovascular disease as the leading cause of death. Post-acute coronary syndrome, SMI patients, including bipolar disorder, often face poor prognosis and lower percutaneous coronary intervention (PCI) rates. We aimed to assess PCI prevalence and outcomes in patients with bipolar disorder.
Methods: We analyzed the National Inpatient Sample data from 2016-2019, identifying 4,483,509 hospitalized adults with myocardial infarction (MI). These hospitalizations were further stratified based on the presence or absence of bipolar disorder using ICD-10 codes. A multivariate regression model was used to adjust for confounders and analyze the variables.
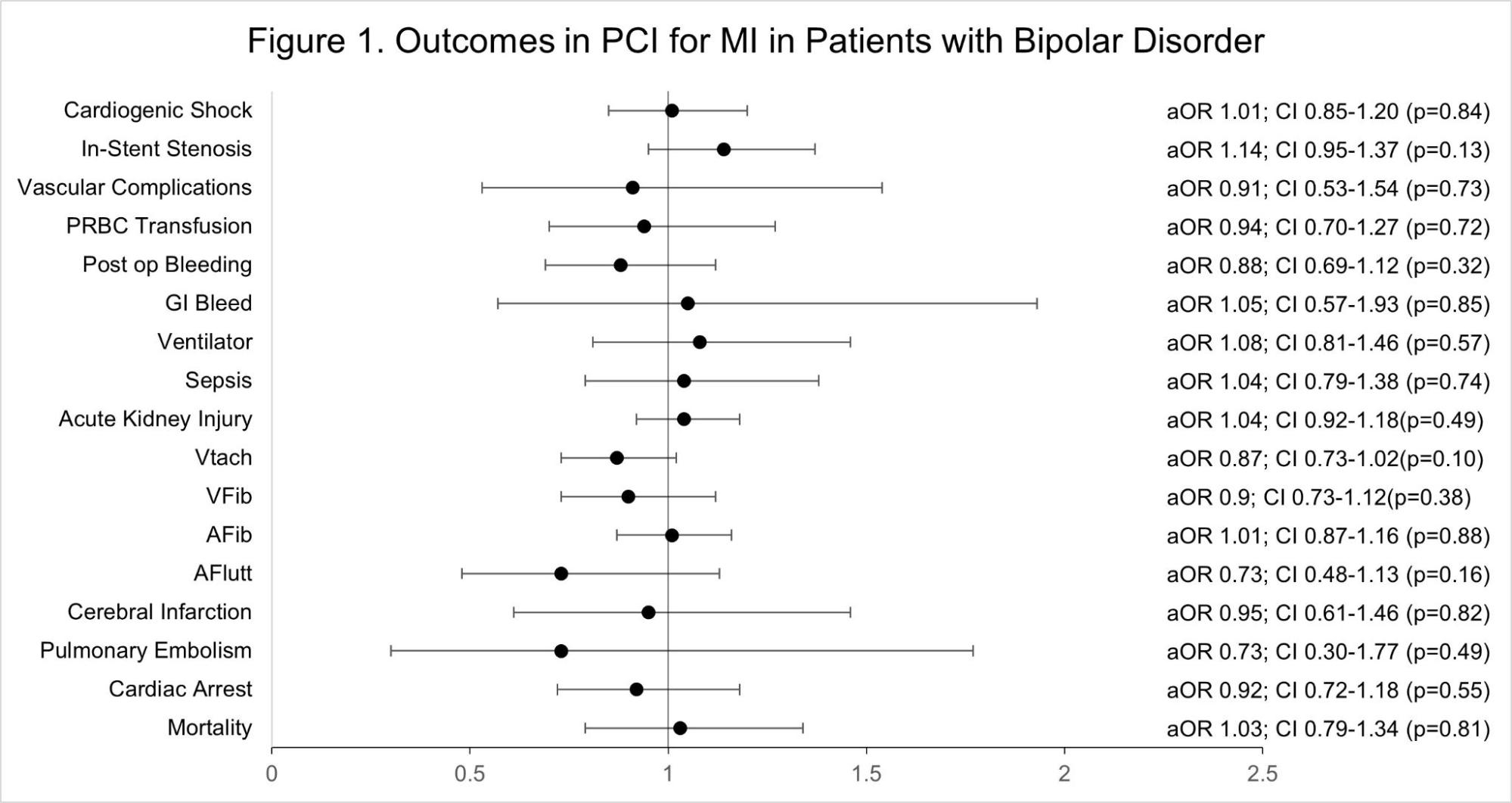
Results: Out of 142,420,378 hospitalizations, 4,483,509 (3.15%) were identified with MI. Among those with MI, 1,221,030 (27.24%) underwent PCI. PCI rates were higher among MI patients without bipolar disorder compared to those with bipolar disorder (27.4% vs. 20%; p<0.001). Figure 1 depicts the Forest plot for multivariate analysis of complications. The length of stay (LOS) in patients with bipolar disorder was 0.24 days longer (p=0.02) on univariate analysis. However, on multivariate analysis, adjusted for patient demographics, comorbidities, and hospital characteristics, the difference in LOS was not statistically significant. Similarly, when adjusted for these variables, bipolar disorder patients who underwent PCI had no statistical difference in terms of mortality (adjusted odds ratio [AOR] 1.03; CI 0.79-1.34; p=0.81) and In-stent stenosis (ISR) (AOR 1.14; CI 0.95-1.37; p=0.13). Although bipolar disorder patients incurred slightly higher total hospitalization costs ($116,931 vs. $116,381 for those without bipolar disorder), this difference was not statistically significant (p = 0.812).
Conclusion: Our study reveals a significant healthcare disparity: despite comparable outcomes in mortality, in-stent stenosis, and other complications, individuals with bipolar disorder are less likely to undergo PCI following MI. These findings underscore the need for targeted interventions to ensure equitable healthcare access for all patients.
Methods: We analyzed the National Inpatient Sample data from 2016-2019, identifying 4,483,509 hospitalized adults with myocardial infarction (MI). These hospitalizations were further stratified based on the presence or absence of bipolar disorder using ICD-10 codes. A multivariate regression model was used to adjust for confounders and analyze the variables.
Results: Out of 142,420,378 hospitalizations, 4,483,509 (3.15%) were identified with MI. Among those with MI, 1,221,030 (27.24%) underwent PCI. PCI rates were higher among MI patients without bipolar disorder compared to those with bipolar disorder (27.4% vs. 20%; p<0.001). Figure 1 depicts the Forest plot for multivariate analysis of complications. The length of stay (LOS) in patients with bipolar disorder was 0.24 days longer (p=0.02) on univariate analysis. However, on multivariate analysis, adjusted for patient demographics, comorbidities, and hospital characteristics, the difference in LOS was not statistically significant. Similarly, when adjusted for these variables, bipolar disorder patients who underwent PCI had no statistical difference in terms of mortality (adjusted odds ratio [AOR] 1.03; CI 0.79-1.34; p=0.81) and In-stent stenosis (ISR) (AOR 1.14; CI 0.95-1.37; p=0.13). Although bipolar disorder patients incurred slightly higher total hospitalization costs ($116,931 vs. $116,381 for those without bipolar disorder), this difference was not statistically significant (p = 0.812).
Conclusion: Our study reveals a significant healthcare disparity: despite comparable outcomes in mortality, in-stent stenosis, and other complications, individuals with bipolar disorder are less likely to undergo PCI following MI. These findings underscore the need for targeted interventions to ensure equitable healthcare access for all patients.
More abstracts on this topic:
Platelet Transcriptomic for Coronary Artery Disease Diagnosis Using Machine Learning
Zhu Wenjun, Zhao Xin, Zhong Yao, Yang Qing, Zhou Xin
A Randomized Clinical Trial Evaluating Vitamin D Normalization on Major Adverse Cardiovascular-Related Events Among Acute Coronary Syndrome Patients: The TARGET-D TrialMay Heidi, Colipi Dominique, Whiting Tyler, Muhlestein Joseph, Le Viet, Anderson Jeffrey, Babcock Daniel, Wayman Libby, Bair Tami, Knight Stacey, Knowlton Kirk, Iverson Leslie