Final ID: Sa2160
Educational Attainment Level and Risk of Mortality and Cardiopulmonary Outcomes in High-Risk Cardiovascular Disease Patients: The INVESTED Trial
Abstract Body (Do not enter title and authors here): Background
Social determinants, such as educational attainment level (EAL), are indicators of socioeconomic status and have been shown to be inversely related with adverse health outcomes. However, the association between EAL and risk of cardio-pulmonary events in heart failure (HF) and myocardial infarction (MI) survivors has not been extensively investigated.
Methods
In the INVESTED trial, 5260 patients from the US and Canada with recent HF or MI hospitalization were randomized 1:1 to high-dose trivalent or standard-dose quadrivalent influenza vaccine from Sep 2016 to Jan 2019. We examined the association between EAL and risk of adverse clinical outcomes for each participant across all enrolling seasons using Cox models adjusted for treatment assignment and clinically relevant confounders and stratified by trial entry year. Participants were categorized by EAL (high school or less [HS], post-high school or trade [post-HS/T], and college or more [Col+]).
Results
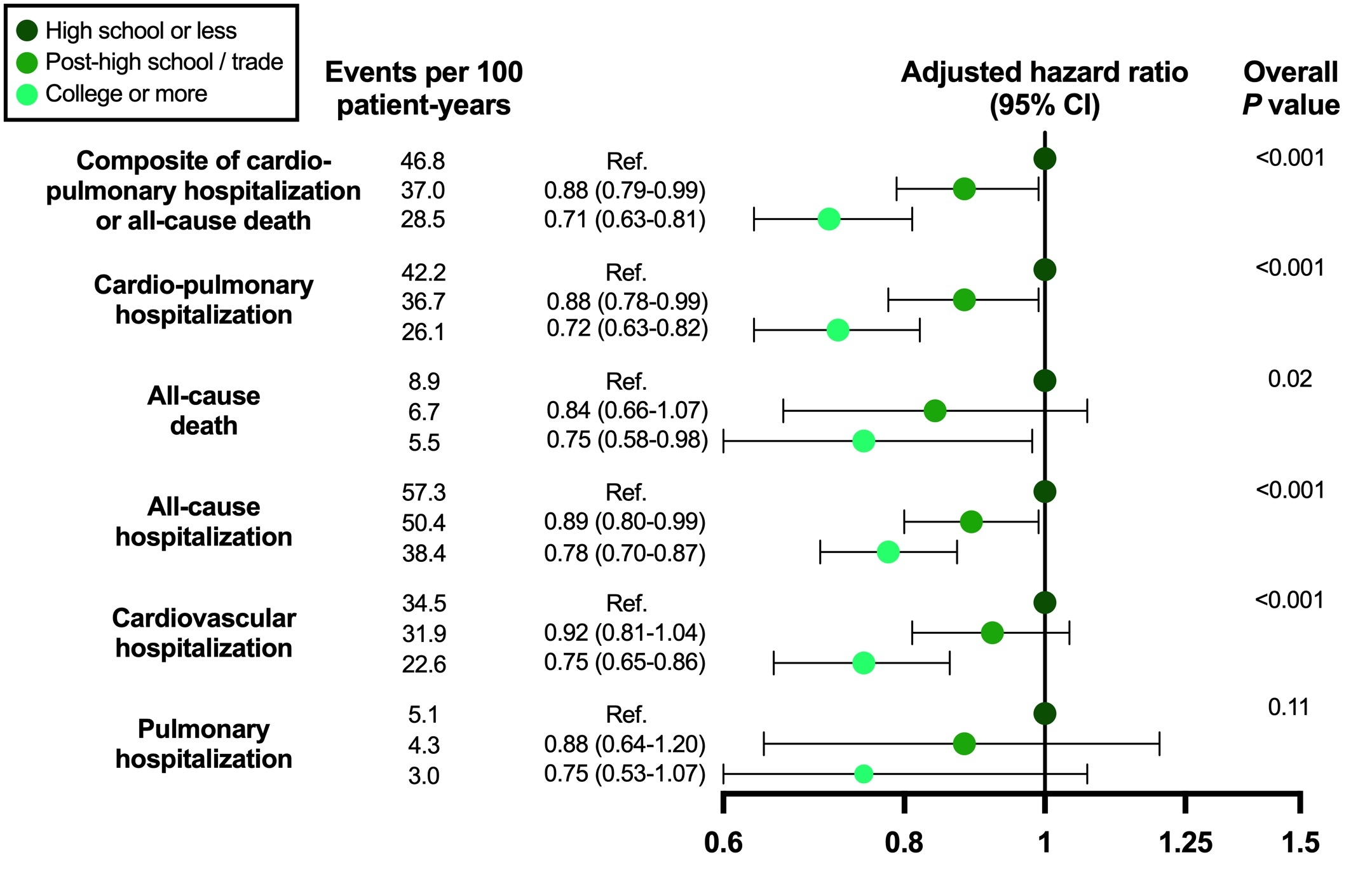
Of the 4,912 participants (mean age: 65.5 years, 28% females, 80% White, 39% with MI and 61% with HF hospitalization as qualifying event) with EAL information, 43% were in the HS group, 28% were in the post-HS/T group, and 29% were in the Col+ group. At baseline, those with higher EAL were more likely to be White or Asian, be married/with long-term partner, have higher left ventricular ejection fraction, have lower NYHA class, and less likely to have cardiovascular comorbidities and risk factors than those with lower EAL. During follow-up (median: 9 months [6-16]), 1,706 (35%) participants experienced the composite of all-cause death or cardiopulmonary hospitalization. Compared to HS, higher EAL was associated with a stepwise decrease in the risk of the composite outcome (post-HS/T: HR: 0.88 95%CI: [0.79-0.99]; Col+: HR: 0.71 95%CI: [0.63-0.81], overall p-value <0.001). A similar protective effect of higher EAL was observed for additional adverse clinical outcomes (Figure).
Conclusion
High EAL is independently associated with a decreased risk of adverse clinical outcomes in patients with high-risk cardiovascular disease, highlighting the need to consider EAL in risk assessment and target additional resources towards those with low EAL to improve prognosis.
Social determinants, such as educational attainment level (EAL), are indicators of socioeconomic status and have been shown to be inversely related with adverse health outcomes. However, the association between EAL and risk of cardio-pulmonary events in heart failure (HF) and myocardial infarction (MI) survivors has not been extensively investigated.
Methods
In the INVESTED trial, 5260 patients from the US and Canada with recent HF or MI hospitalization were randomized 1:1 to high-dose trivalent or standard-dose quadrivalent influenza vaccine from Sep 2016 to Jan 2019. We examined the association between EAL and risk of adverse clinical outcomes for each participant across all enrolling seasons using Cox models adjusted for treatment assignment and clinically relevant confounders and stratified by trial entry year. Participants were categorized by EAL (high school or less [HS], post-high school or trade [post-HS/T], and college or more [Col+]).
Results
Of the 4,912 participants (mean age: 65.5 years, 28% females, 80% White, 39% with MI and 61% with HF hospitalization as qualifying event) with EAL information, 43% were in the HS group, 28% were in the post-HS/T group, and 29% were in the Col+ group. At baseline, those with higher EAL were more likely to be White or Asian, be married/with long-term partner, have higher left ventricular ejection fraction, have lower NYHA class, and less likely to have cardiovascular comorbidities and risk factors than those with lower EAL. During follow-up (median: 9 months [6-16]), 1,706 (35%) participants experienced the composite of all-cause death or cardiopulmonary hospitalization. Compared to HS, higher EAL was associated with a stepwise decrease in the risk of the composite outcome (post-HS/T: HR: 0.88 95%CI: [0.79-0.99]; Col+: HR: 0.71 95%CI: [0.63-0.81], overall p-value <0.001). A similar protective effect of higher EAL was observed for additional adverse clinical outcomes (Figure).
Conclusion
High EAL is independently associated with a decreased risk of adverse clinical outcomes in patients with high-risk cardiovascular disease, highlighting the need to consider EAL in risk assessment and target additional resources towards those with low EAL to improve prognosis.
More abstracts on this topic:
COVID-19 Vaccine-Induced Cardiac Inflammation: A Review of 103 Cases and Appraisal of VAERS Database
Padda Inderbir, Sethi Yashendra, Choudhary Khushal, Malhi Amarveer, Bharaj Inderjeet Singh, Fabian Daniel, Farid Meena
β1 Adrenergic Receptor Autoantibodies Promote Heart Failure Though Activation of Prostaglandin E2 Receptor EP1/Phosphodiesterase 4B PathwayCao Ning, Qiu Hui, Li Hongwei