Final ID: Mo4169
Isolated Tricuspid Replacement versus Repair among Medicare Beneficiaries
Abstract Body (Do not enter title and authors here): Background: Evidence is limited regarding mid-term outcomes following isolated tricuspid operations for tricuspid regurgitation at the population level.
Objective: This study aimed to compare the mid-term outcomes following isolated tricuspid valve replacement versus repair using contemporary data.
Methods: We analyzed the national data on Medicare beneficiaries aged ≥65 who underwent isolated tricuspid valve replacement or repair between January 2016 and December 2020. The primary outcome was mid-term (up to 3 years) all-cause mortality. The secondary outcomes included mid-term major adverse cardiovascular events (MACE) and heart failure hospitalizations, as well as in-hospital permanent pacemaker implantation rates. MACE comprised all-cause mortality, heart failure hospitalization, stroke, and tricuspid reoperations. A propensity score-matching analysis was conducted to compare the two groups.
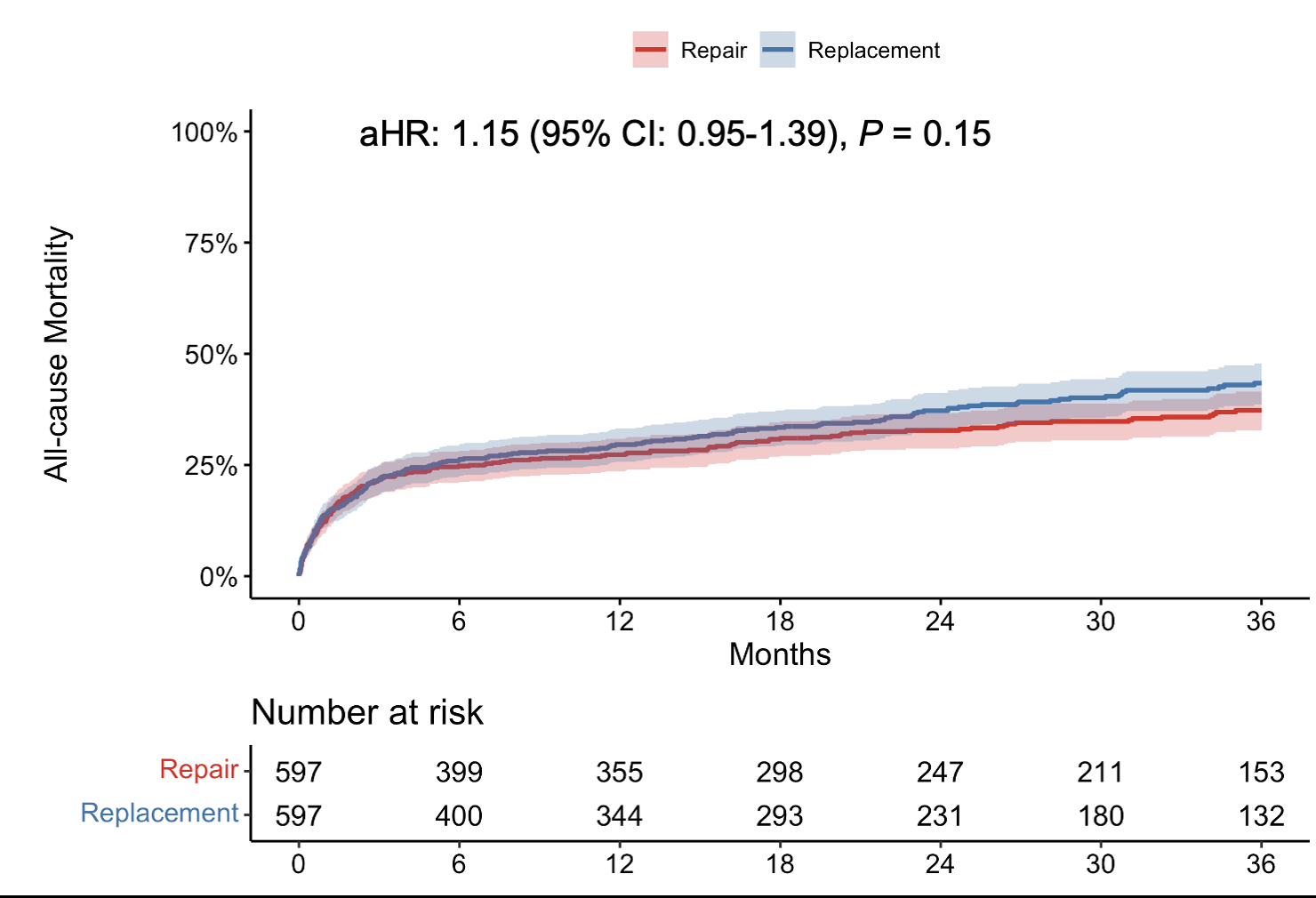
Results: A total of 1,693 patients were included (replacement= 655 patients, repair= 1,038 patients). In the matched cohort (597 patients in each group), the overall mortality and MACE were 40% and 47% at 3 years, respectively. Tricuspid valve replacement was associated with similar all-cause mortality in comparison to repair (adjusted hazard ratio [HR], 1.15; 95% confidence interval [CI], 0.95-1.39; P=0.15). Similarly, the rates of MACE and heart failure hospitalizations were similar (adjusted HR, 1.10; 95% CI, 0.93-1.32, P=0.27; subdistribution HR, 1.07, 95% CI, 0.75-1.54, P=0.69, respectively) between these two procedures. Patients undergoing replacement required permanent pacemaker implantations more frequently (25.4% vs. 12.4%; P<0.001).
Conclusions: Isolated surgical tricuspid valve replacement was associated with similar clinical outcomes compared to repair, except for permanent pacemaker implantation rates. The overall high mid-term mortality and morbidity with either treatment highlight the need for better options and further research to optimize the indication and timing of intervention.
Objective: This study aimed to compare the mid-term outcomes following isolated tricuspid valve replacement versus repair using contemporary data.
Methods: We analyzed the national data on Medicare beneficiaries aged ≥65 who underwent isolated tricuspid valve replacement or repair between January 2016 and December 2020. The primary outcome was mid-term (up to 3 years) all-cause mortality. The secondary outcomes included mid-term major adverse cardiovascular events (MACE) and heart failure hospitalizations, as well as in-hospital permanent pacemaker implantation rates. MACE comprised all-cause mortality, heart failure hospitalization, stroke, and tricuspid reoperations. A propensity score-matching analysis was conducted to compare the two groups.
Results: A total of 1,693 patients were included (replacement= 655 patients, repair= 1,038 patients). In the matched cohort (597 patients in each group), the overall mortality and MACE were 40% and 47% at 3 years, respectively. Tricuspid valve replacement was associated with similar all-cause mortality in comparison to repair (adjusted hazard ratio [HR], 1.15; 95% confidence interval [CI], 0.95-1.39; P=0.15). Similarly, the rates of MACE and heart failure hospitalizations were similar (adjusted HR, 1.10; 95% CI, 0.93-1.32, P=0.27; subdistribution HR, 1.07, 95% CI, 0.75-1.54, P=0.69, respectively) between these two procedures. Patients undergoing replacement required permanent pacemaker implantations more frequently (25.4% vs. 12.4%; P<0.001).
Conclusions: Isolated surgical tricuspid valve replacement was associated with similar clinical outcomes compared to repair, except for permanent pacemaker implantation rates. The overall high mid-term mortality and morbidity with either treatment highlight the need for better options and further research to optimize the indication and timing of intervention.
More abstracts on this topic:
A Remote Patient Care Heart Failure Program Drives Improved Clinical Outcomes and Reduced Healthcare Cost and Utilization
Feldman David, Reynolds Spencer, Curnow Randall, Cunningham Eve, Feldman Theodore, Fudim Marat
Cell senescence and abnormal autophagy flux contribute to mitral valve degeneration in Barlow diseaseTang Qiyu, Chester Adrian, Macrae Vicky, Corcoran Brendan