Final ID: MDP1227
Association between Age at Menarche and Age at Onset of Angina Pectoris: An Analysis of NHANES Data from 2017-2020
Abstract Body (Do not enter title and authors here): Background:
There is suspicion that estrogen may protect against atherosclerosis. Women who experience menarche earlier, and thus have earlier estrogen exposure, might develop atherosclerosis later. The relationship between menarche age and the onset of angina pectoris, a symptom of coronary artery disease, remains unknown.
Goal:
This study aims to find the correlation between menarche age and the onset age of angina pectoris, and the association between early menarche (onset of menarche ≤ 10 y/o) and early onset of angina pectoris (onset of angina pectoris ≤ 40 y/o).
Methods:
A cross-sectional study using a population from the 2017-2020 National Health and Nutrition Examination Survey (NHANES). The question collects self-reported data on onset of menarche and onset of angina pectoris. The relationship between menarche age and age in onset of angina pectoris was analyzed by linear and logistic regression analysis. Multivariate analysis adjusted for race, age, body mass index (BMI), smoking , diabetes mellitus (DM), hypertension, and dyslipidemia status.
Results:
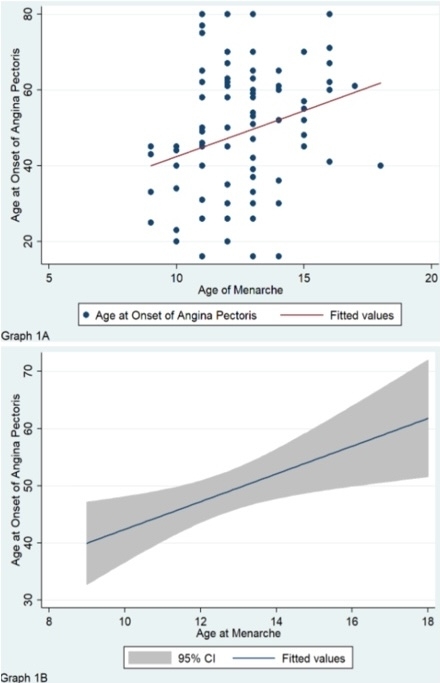
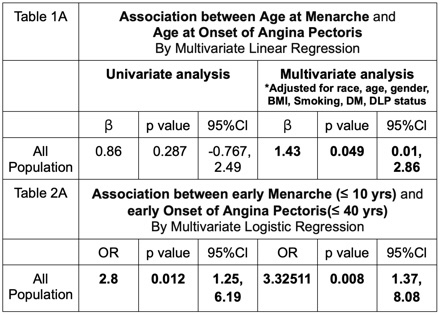
Among 4,816 females who reported their menarche age, 88(1.8 %) have had an angina pectoris. The study involved 82 females who reported both the age of menarche and the age of onset of angina pectoris. The mean ± SD of the age at menarche and the age at onset of angina pectoris was 12.53 ± 1.79 y/o and 51.66 ± 15.16 y/o, respectively. The study found a significant association between the menarche age and the age at onset of angina pectoris. After adjusting for confounders, we found that every 1-year increase in the age of menarche will delay the onset of angina pectoris by 1.43 years, with a 95% CI of 0.01 to 2.86.(Table 1A,Graph 1A-1B)
We also found that early menarche has a significantly increased risk 2.8 times (95%CI: 1.3, 6.2) of early onset of angina pectoris.After adjusting for confounders, the association became even stronger. The odds ratio (OR) increased to 3.3 (95%CI: 1.4, 8.0), indicating that women with early menarche were 3.3 times more likely to experience early angina pectoris compared to those with later menarche.(Table 2A)
Conclusion:
In contrast to our hypothesis, age at menarche is positively associated with onset of angina pectoris. The earlier onset of menarche is linked to the earlier onset of angina pectoris. We suspected that factors beyond estrogen levels may contribute to this unexpected finding. Additional studies are needed to examine the cause of this correlation.
There is suspicion that estrogen may protect against atherosclerosis. Women who experience menarche earlier, and thus have earlier estrogen exposure, might develop atherosclerosis later. The relationship between menarche age and the onset of angina pectoris, a symptom of coronary artery disease, remains unknown.
Goal:
This study aims to find the correlation between menarche age and the onset age of angina pectoris, and the association between early menarche (onset of menarche ≤ 10 y/o) and early onset of angina pectoris (onset of angina pectoris ≤ 40 y/o).
Methods:
A cross-sectional study using a population from the 2017-2020 National Health and Nutrition Examination Survey (NHANES). The question collects self-reported data on onset of menarche and onset of angina pectoris. The relationship between menarche age and age in onset of angina pectoris was analyzed by linear and logistic regression analysis. Multivariate analysis adjusted for race, age, body mass index (BMI), smoking , diabetes mellitus (DM), hypertension, and dyslipidemia status.
Results:
Among 4,816 females who reported their menarche age, 88(1.8 %) have had an angina pectoris. The study involved 82 females who reported both the age of menarche and the age of onset of angina pectoris. The mean ± SD of the age at menarche and the age at onset of angina pectoris was 12.53 ± 1.79 y/o and 51.66 ± 15.16 y/o, respectively. The study found a significant association between the menarche age and the age at onset of angina pectoris. After adjusting for confounders, we found that every 1-year increase in the age of menarche will delay the onset of angina pectoris by 1.43 years, with a 95% CI of 0.01 to 2.86.(Table 1A,Graph 1A-1B)
We also found that early menarche has a significantly increased risk 2.8 times (95%CI: 1.3, 6.2) of early onset of angina pectoris.After adjusting for confounders, the association became even stronger. The odds ratio (OR) increased to 3.3 (95%CI: 1.4, 8.0), indicating that women with early menarche were 3.3 times more likely to experience early angina pectoris compared to those with later menarche.(Table 2A)
Conclusion:
In contrast to our hypothesis, age at menarche is positively associated with onset of angina pectoris. The earlier onset of menarche is linked to the earlier onset of angina pectoris. We suspected that factors beyond estrogen levels may contribute to this unexpected finding. Additional studies are needed to examine the cause of this correlation.
More abstracts on this topic:
12-lead electrocardiograms predict adverse cardiovascular outcomes of emergency department patients
Haimovich Julian, Kolossvary Marton, Alam Ridwan, Padros I Valls Raimon, Lu Michael, Aguirre Aaron
Coronary Microvascular Disease Modulates Long-Term Outcomes in Myocardial Infarction with Non-Obstructive Coronary ArteriesCarrington Justin, Nogami Kai, Prasad Abhiram, Gulati Rajiv, Lerman Amir, Raphael Claire