Final ID: Su3059
Overview of Direct Oral Anticoagulation Trends in the North Bronx: Patient and Systemic Factors Contributing to Medication Nonadherence
Abstract Body (Do not enter title and authors here): Introduction: Anticoagulation nonadherence has historically been attributed to myriad factors in patient populations worldwide. While direct oral anticoagulants (DOACs) have demonstrated advantages such as less routine monitoring and fewer interactions with other medications over other anticoagulant classes, nonadherence persists and the underlying contributors vary by geography. The goal of this retrospective review was to highlight on the patient and systemic characteristics associated with DOAC nonadherence in the North Bronx.
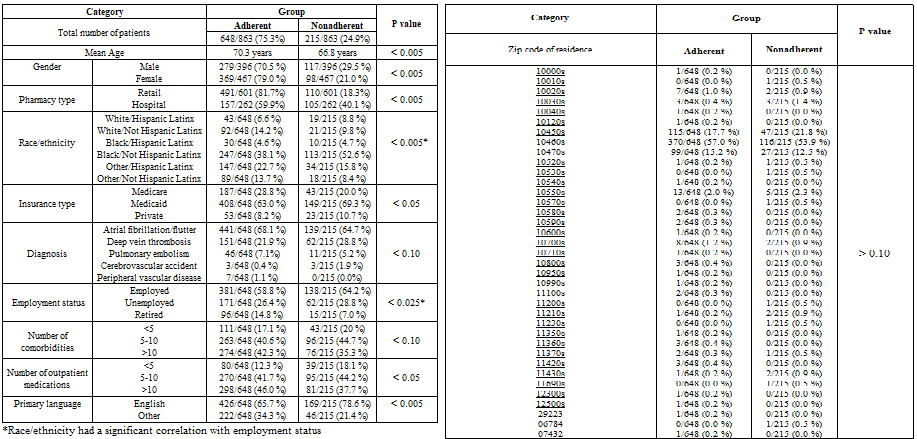
Methods: This review used records between 2017-2024 from two major hospital centers in the North Bronx. Patients receiving outpatient primary care and active DOAC therapy were included in the analysis. Adherence and nonadherence groups were determined based on prescription fill status and MD documentation of medication intake patterns. The groups were compared in the categories of age, gender, race, ethnicity, insurance type, diagnosis, pharmacy type, employment status, comorbidity burden, outpatient medications, primary language, and zip code. Chi square analysis was done between the categories and outcomes as well as between categories. A p value of < 0.05 was deemed significant.
Results: The cohort had 863 patients with nonadherence of 24.9%. The adherent group's mean age was higher than that of the nonadherent (70.3 years vs 66.8 years, p < 0.005). Females were more adherent than males (79.0% vs 70.5%, p < 0.005). The adherent group was also more likely to be receiving DOAC from a retail pharmacy than from a hospital pharmacy (81.7% vs 59.9%, p < 0.005). The nonadherent group was more likely to be insured under medicaid (69.3% vs 63.0%, p < 0.005) and to be taking fewer than 10 outpatient medications (62.3% vs 54.0%, p < 0.05). English was the primary language of more patients in the nonadherent group (78.6% vs 65.7%, p < 0.005).
Conclusion: DOAC nonadherence in the North Bronx correlates with patient age, gender, pharmacy type, insurance type, number of outpatient medications, and primary language. Nonadherence does not correlate with comorbidity burden, diagnosis, or zip code. Associations with race/ethnicity and employment status were uncertain and warrant further study.
Methods: This review used records between 2017-2024 from two major hospital centers in the North Bronx. Patients receiving outpatient primary care and active DOAC therapy were included in the analysis. Adherence and nonadherence groups were determined based on prescription fill status and MD documentation of medication intake patterns. The groups were compared in the categories of age, gender, race, ethnicity, insurance type, diagnosis, pharmacy type, employment status, comorbidity burden, outpatient medications, primary language, and zip code. Chi square analysis was done between the categories and outcomes as well as between categories. A p value of < 0.05 was deemed significant.
Results: The cohort had 863 patients with nonadherence of 24.9%. The adherent group's mean age was higher than that of the nonadherent (70.3 years vs 66.8 years, p < 0.005). Females were more adherent than males (79.0% vs 70.5%, p < 0.005). The adherent group was also more likely to be receiving DOAC from a retail pharmacy than from a hospital pharmacy (81.7% vs 59.9%, p < 0.005). The nonadherent group was more likely to be insured under medicaid (69.3% vs 63.0%, p < 0.005) and to be taking fewer than 10 outpatient medications (62.3% vs 54.0%, p < 0.05). English was the primary language of more patients in the nonadherent group (78.6% vs 65.7%, p < 0.005).
Conclusion: DOAC nonadherence in the North Bronx correlates with patient age, gender, pharmacy type, insurance type, number of outpatient medications, and primary language. Nonadherence does not correlate with comorbidity burden, diagnosis, or zip code. Associations with race/ethnicity and employment status were uncertain and warrant further study.
More abstracts on this topic:
Air pollution and Cardiovascular Disease Incidence in a Pooled Analysis of 6 U.S. Cohorts
Leiser Claire, Spalt Elizabeth, Kaufman Joel, Quraishi Sabah, Biggs Mary Lou, Hart Jaime, Sandler Dale, Whitsel Eric, White Alexandra, Young Michael T, Szpiro Adam
Comparison of FAST and BE-FAST Performance Among the General PublicAncheta Selina, Philpot Debra, Reeves Mathew, Witt John, Zachrison Kori, Adeoye Opeolu, Denny Mary Carter, Dunn Mary, Elkind Mitchell, Kleindorfer Dawn, Lane Patricia, Madhok Debbie, Miller-smith Katie, Mohl Stephanie