Final ID: Mo3093
Self-monitoring of Home Blood Pressures Identifies a High Prevalence of White Coat and Masked Hypertension in Cardiac Rehabilitation Patients
Abstract Body (Do not enter title and authors here): Introduction: Hypertension (HTN) is a highly prevalent risk factor that is targeted for the risk reduction and recovery of patients attending cardiac rehabilitation (CR) after a CV event. Self-measured home blood pressure monitoring (SM-BPs) is becoming a main approach for BP management, but how SM-BPs relate to BPs measured during in-center CR participation (CR-BPs) has not been previously reported.
Objective: To compare concordance between SM-BPs and CR-BPs during the rehabilitation of high-risk CV patients.
Methods: We studied 143 CR patients with SM-BPs in addition to CR-BPs. Patients were classified as having HTN if their starting BP in CR ≥130/80 (average of first 3 sessions). The prevalence of white coat (WC) and masked HTN were determined based on concomitant home BP readings. Concordance of SM-BP and CR-BP trajectories over time was determined using a linear mixed-effects model in 90 patients (63%) who had at least 2 weeks of concomitant measurements.
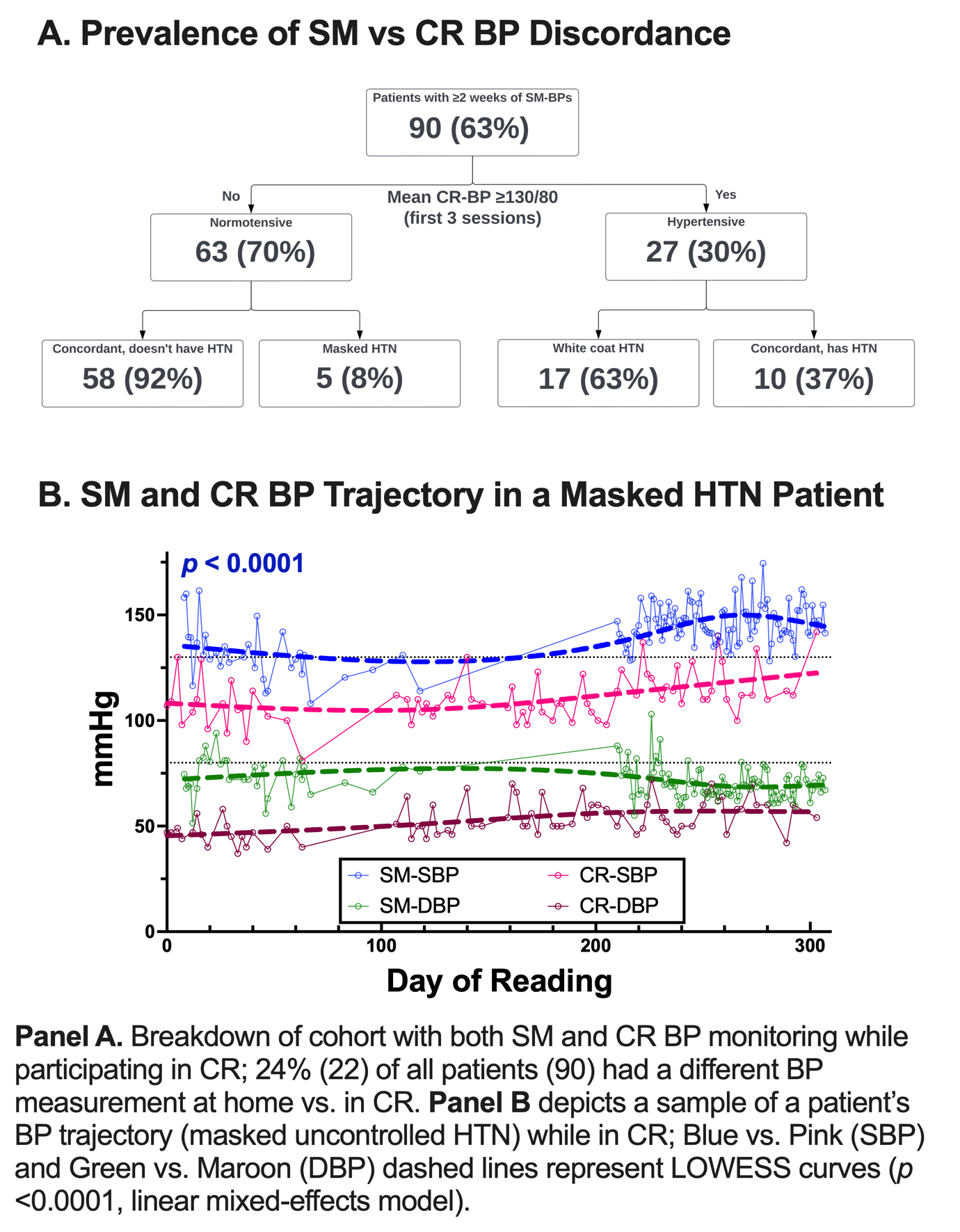
Results: Of the 90 included patients (65±12 (SD) years, 33% female, 34% non-White), 77%, 41%, 24%, 23%, 37% and 22% had a history of HTN, any tobacco use, DMT2, HF, CAD, and PVD, respectively. Of the 30% of patients with high CR-BP initially, 17 (63%) were found to have WC HTN and 8% of normotensive patients had masked HTN (Figure 1, panel A). Twenty-nine patients (32%) had statistically significant discordance between SM-BPs and CR-BPs throughout CR participation (p < 0.05; Figure 1, panel B).
Conclusion: To the best of our knowledge, this case series represents the 1st report of concomitant SM-BP and CR-BP trajectories over time. We identified white coat HTN (63%) among hypertensive patients and masked uncontrolled HTN (8%) among normotensive patients. Masked HTN may contribute to missing a prevention target whereas WC HTN may contribute to medical overtreatment of BP while adopting healthy lifestyle modifications. Not surprisingly, BP readings changed over time and 32% of patients had significant discordance between home and center, which could inform rational therapies in CR if recognized in a timely manner. We propose that SM-BPs should be rigorously and systematically measured during CR to further guide BP management in high-risk CV patients.
Objective: To compare concordance between SM-BPs and CR-BPs during the rehabilitation of high-risk CV patients.
Methods: We studied 143 CR patients with SM-BPs in addition to CR-BPs. Patients were classified as having HTN if their starting BP in CR ≥130/80 (average of first 3 sessions). The prevalence of white coat (WC) and masked HTN were determined based on concomitant home BP readings. Concordance of SM-BP and CR-BP trajectories over time was determined using a linear mixed-effects model in 90 patients (63%) who had at least 2 weeks of concomitant measurements.
Results: Of the 90 included patients (65±12 (SD) years, 33% female, 34% non-White), 77%, 41%, 24%, 23%, 37% and 22% had a history of HTN, any tobacco use, DMT2, HF, CAD, and PVD, respectively. Of the 30% of patients with high CR-BP initially, 17 (63%) were found to have WC HTN and 8% of normotensive patients had masked HTN (Figure 1, panel A). Twenty-nine patients (32%) had statistically significant discordance between SM-BPs and CR-BPs throughout CR participation (p < 0.05; Figure 1, panel B).
Conclusion: To the best of our knowledge, this case series represents the 1st report of concomitant SM-BP and CR-BP trajectories over time. We identified white coat HTN (63%) among hypertensive patients and masked uncontrolled HTN (8%) among normotensive patients. Masked HTN may contribute to missing a prevention target whereas WC HTN may contribute to medical overtreatment of BP while adopting healthy lifestyle modifications. Not surprisingly, BP readings changed over time and 32% of patients had significant discordance between home and center, which could inform rational therapies in CR if recognized in a timely manner. We propose that SM-BPs should be rigorously and systematically measured during CR to further guide BP management in high-risk CV patients.
More abstracts on this topic:
An Effective mHealth Intervention to Close the Guideline-to-Practice Gap in Hypertension Treatment: mGlide RCT
Lakshminarayan Kamakshi, Murray Thomas, Mccarthy Teresa, Luepker Russell, Drawz Paul, Streib Christopher, Everson-rose Susan, Connett John, Westberg Sarah
Basic Tools and Big Impact: A Tele-assisted Home-based Cardiac Rehabilitation Model for LMICsMukherjee Anirudh, Duggal Bhanu, Rathore Sudhir, Singh Meenu