Final ID: Mo4089
Hybrid Coronary Revascularization versus Traditional Coronary Artery Bypass Grafting for Left Main Disease
Abstract Body (Do not enter title and authors here): Background:
The current guideline-recommended intervention for left main (LM) disease is coronary artery bypass grafting (CABG). Hybrid coronary revascularization (HCR) combines robotic coronary artery bypass and percutaneous coronary intervention (PCI) and offers a less invasive approach for patients with LM and multivessel coronary artery disease. We aim to compare clinical outcomes at 30 days, 6 months and 1 year between HCR and CABG in patients with LM disease.
Methods:
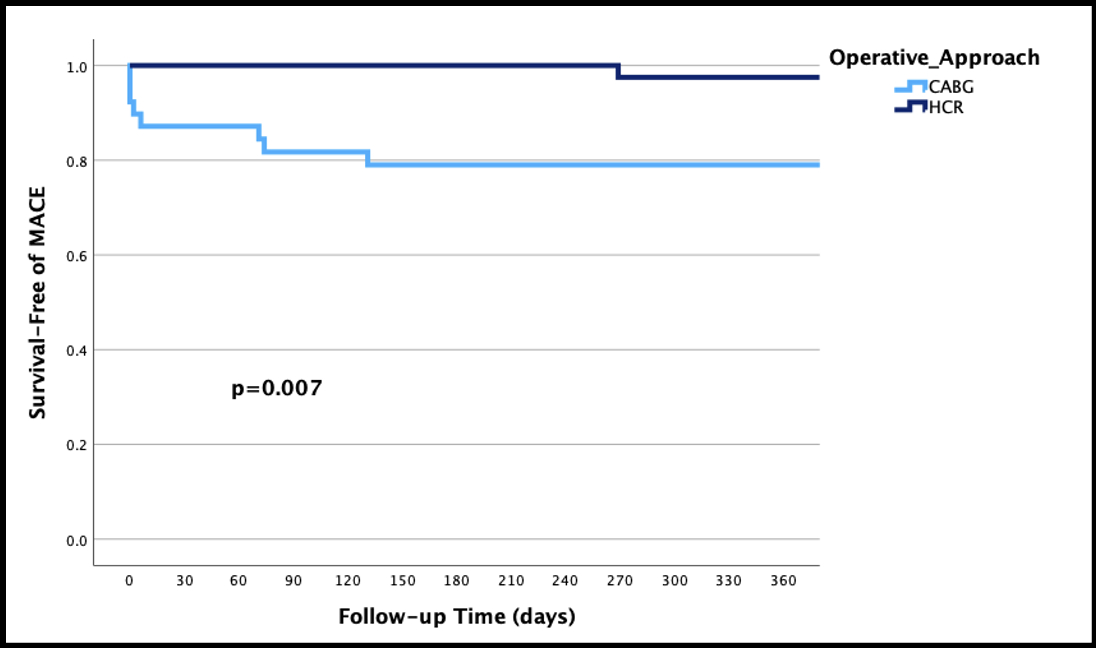
We retrospectively screened 761 patients who underwent bypass for LM disease between 2019 and 2023 at a single institution. A total of 118 patients who underwent either HCR (n=59) or CABG (n=59) were included after propensity matching for baseline characteristics. The primary endpoint was major adverse cardiovascular events (MACE), defined as death, myocardial infarction, repeat revascularization and stroke, at 30 days, 6 months and 1 year, which was assessed using chi-squared tests. Secondary outcomes are individual components of MACE at 30 days, 6 months and 1 year. Kaplan-Meier curves were used to visualize the difference in 1-year cumulative MACE-free survival across groups coupled with a log-rank test.
Results:
The mean age was 68.93±11 years for HCR patients and 68.41±10.11 years for CABG patients (p=0.394). SYNTAX score was high (> 33) for 49.1% of HCR patients and 67.3% of CABG patients (p=0.15). Hospital length of stay was shorter for HCR compared to CABG (4.07 ± 1.21 days vs. 7.58 ± 7.71 days, p<0.001). MACE events were significantly lower in the HCR group at 30 days (0% vs 10.2%; p=0.01), 6 months (0% vs 17%; p=0.002) and 1 year (2.4% vs 20.5%; p=0.01). The cumulative MACE-free survival at 1 year was significantly higher in the HCR group (p=0.007). There were no significant differences in secondary outcomes at any time point with the exception of lower repeat revascularization at 6 months in the HCR group (0% vs 10.9%; p=0.02).
Conclusion:
This retrospective study demonstrates that HCR is a viable alternative to CABG for LM disease. While randomized clinical trial data is still needed, this less invasive approach is a promising treatment strategy for patients with high surgical risk.
The current guideline-recommended intervention for left main (LM) disease is coronary artery bypass grafting (CABG). Hybrid coronary revascularization (HCR) combines robotic coronary artery bypass and percutaneous coronary intervention (PCI) and offers a less invasive approach for patients with LM and multivessel coronary artery disease. We aim to compare clinical outcomes at 30 days, 6 months and 1 year between HCR and CABG in patients with LM disease.
Methods:
We retrospectively screened 761 patients who underwent bypass for LM disease between 2019 and 2023 at a single institution. A total of 118 patients who underwent either HCR (n=59) or CABG (n=59) were included after propensity matching for baseline characteristics. The primary endpoint was major adverse cardiovascular events (MACE), defined as death, myocardial infarction, repeat revascularization and stroke, at 30 days, 6 months and 1 year, which was assessed using chi-squared tests. Secondary outcomes are individual components of MACE at 30 days, 6 months and 1 year. Kaplan-Meier curves were used to visualize the difference in 1-year cumulative MACE-free survival across groups coupled with a log-rank test.
Results:
The mean age was 68.93±11 years for HCR patients and 68.41±10.11 years for CABG patients (p=0.394). SYNTAX score was high (> 33) for 49.1% of HCR patients and 67.3% of CABG patients (p=0.15). Hospital length of stay was shorter for HCR compared to CABG (4.07 ± 1.21 days vs. 7.58 ± 7.71 days, p<0.001). MACE events were significantly lower in the HCR group at 30 days (0% vs 10.2%; p=0.01), 6 months (0% vs 17%; p=0.002) and 1 year (2.4% vs 20.5%; p=0.01). The cumulative MACE-free survival at 1 year was significantly higher in the HCR group (p=0.007). There were no significant differences in secondary outcomes at any time point with the exception of lower repeat revascularization at 6 months in the HCR group (0% vs 10.9%; p=0.02).
Conclusion:
This retrospective study demonstrates that HCR is a viable alternative to CABG for LM disease. While randomized clinical trial data is still needed, this less invasive approach is a promising treatment strategy for patients with high surgical risk.
More abstracts on this topic:
A Shocking Development After Peripheral Arterial Intervention
Aggarwal Devika, Badar Mustanser, Gowda Ramesh
An Unusual Presentation of Cerebellar Stroke Following the Removal of Microaxial Flow PumpLiu Zi Qian, Alsheikh-kassim Mohammad, Karpenos Joseph, Frodey Kevin