Final ID: Su3040
Trends and Disparities in Mortality Due to Thoracic Aortic Aneurysm in Patients in the United States from 1999 to 2020
Abstract Body (Do not enter title and authors here):
Background
Thoracic aortic aneurysms (TAA) impact approximately 6 to 10 individuals per 100,000 people, though the actual prevalence is likely higher due to frequent asymptomatic presentations, posing a challenge for early diagnosis. The rupture of these aneurysms presents a significant risk, resulting in an estimated 30,000 deaths annually in the United States alone. This emphasizes the urgent need for enhanced detection and treatment strategies. An understanding of trends in TAA mortality is imperative for assessing the efficacy of current approaches, pinpointing vulnerable populations, and ultimately, advancing treatment equity.
Methods
This study utilized death certificates from 1999 to 2020 sourced from the CDC WONDER Database. Deaths among individuals aged 25 years and older attributed to TAA were identified using the International Classification of Diseases, Tenth Revision (ICD-10) codes I71.1 and I71.2. Age-adjusted mortality rates (AAMRs) per 1,000,000 individuals and annual percent change (APC) were computed and stratified based on year, gender, race/ethnicity, and urbanization status.
Results
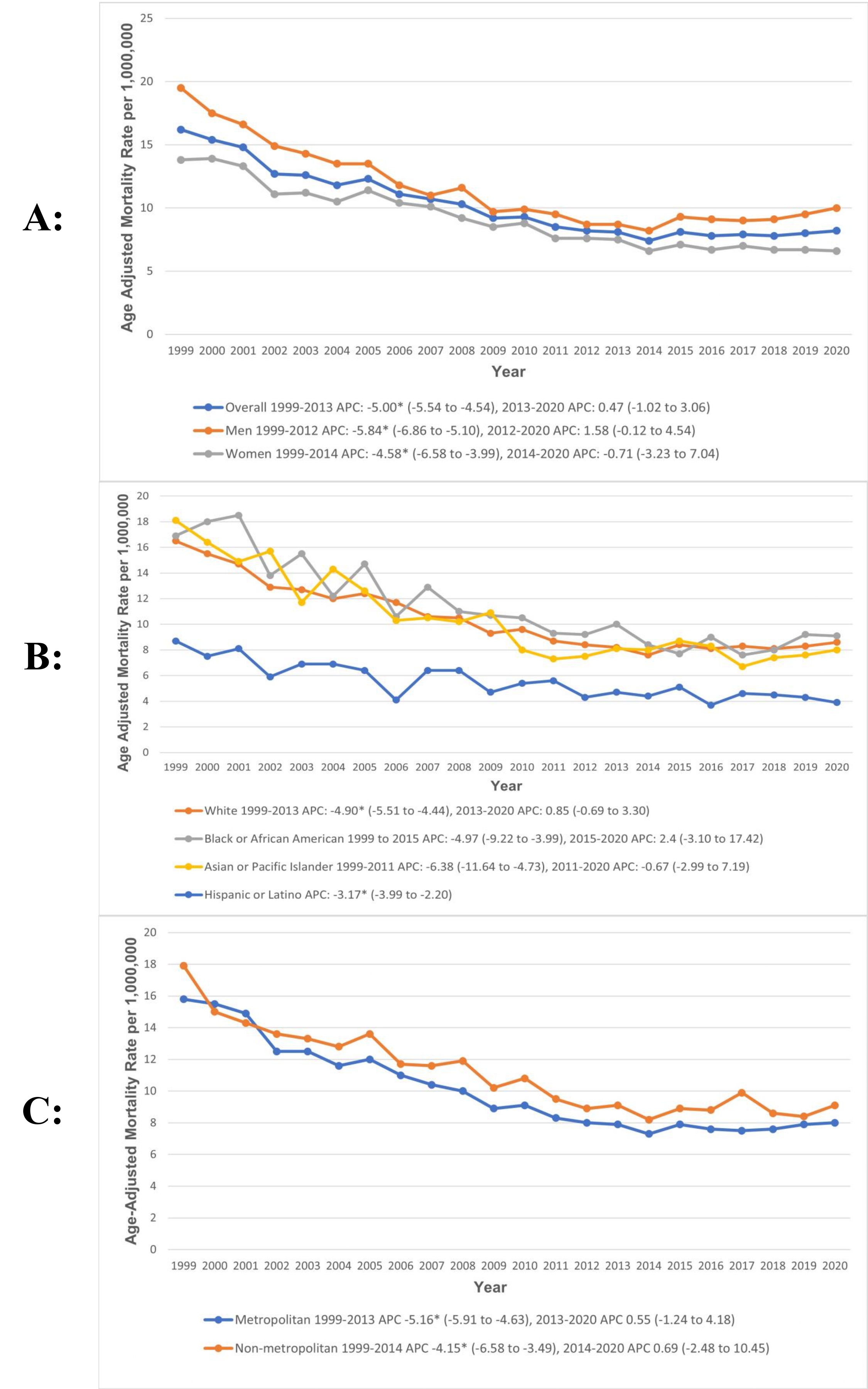
Between 1999 and 2020, 47,136 deaths were reported in patients with TAA. Overall, AAMR decreased from 16.2 to 8.2 per 1,000,000 population between 1999 and 2020, with a significant decline from 1999 to 2013 (APC: -5.00; 95% CI: -5.54 to -4.5), followed by a slight increase from 2013 to 2020 (APC: 0.47; 95% CI: -1.02 to 3.06). Gender-based analysis revealed that men had consistently higher AAMRs than women (men: 11.2; 95% CI: 11 to 11.3; vs. women: 9; 95% CI: 8.9 to 9.1). Moreover, we found that AAMRs were the highest among non-Hispanic African Americans (11; 95% CI: 10.7 to 11.3) followed by non-Hispanic Whites (10.3; 95% CI: 10.2 to 10.4), non-Hispanic Asian or Pacific Islanders (9.5; 95% CI: 9 to 9.9), non-Hispanic American Indian or Alaska Native (7.8; 95% CI: 6.6 to 9), and Hispanic populations (5.2; 95% CI 5 to 5.5). In addition, non-metropolitan areas had higher AAMRs than metropolitan areas (non-metropolitan areas: 11; 95% CI: 10.8 to 11.2; vs. metropolitan: 9.8; 95% CI: 9.7 to 9.9) (Figure 1).
Conclusions
This analysis revealed a significant decline in mortality since 1999 from TAA, with a slight upward trend in recent years. However, disparities persist, with higher AAMRs observed among men, non-Hispanic African Americans, and residents of non-metropolitan areas.
Background
Thoracic aortic aneurysms (TAA) impact approximately 6 to 10 individuals per 100,000 people, though the actual prevalence is likely higher due to frequent asymptomatic presentations, posing a challenge for early diagnosis. The rupture of these aneurysms presents a significant risk, resulting in an estimated 30,000 deaths annually in the United States alone. This emphasizes the urgent need for enhanced detection and treatment strategies. An understanding of trends in TAA mortality is imperative for assessing the efficacy of current approaches, pinpointing vulnerable populations, and ultimately, advancing treatment equity.
Methods
This study utilized death certificates from 1999 to 2020 sourced from the CDC WONDER Database. Deaths among individuals aged 25 years and older attributed to TAA were identified using the International Classification of Diseases, Tenth Revision (ICD-10) codes I71.1 and I71.2. Age-adjusted mortality rates (AAMRs) per 1,000,000 individuals and annual percent change (APC) were computed and stratified based on year, gender, race/ethnicity, and urbanization status.
Results
Between 1999 and 2020, 47,136 deaths were reported in patients with TAA. Overall, AAMR decreased from 16.2 to 8.2 per 1,000,000 population between 1999 and 2020, with a significant decline from 1999 to 2013 (APC: -5.00; 95% CI: -5.54 to -4.5), followed by a slight increase from 2013 to 2020 (APC: 0.47; 95% CI: -1.02 to 3.06). Gender-based analysis revealed that men had consistently higher AAMRs than women (men: 11.2; 95% CI: 11 to 11.3; vs. women: 9; 95% CI: 8.9 to 9.1). Moreover, we found that AAMRs were the highest among non-Hispanic African Americans (11; 95% CI: 10.7 to 11.3) followed by non-Hispanic Whites (10.3; 95% CI: 10.2 to 10.4), non-Hispanic Asian or Pacific Islanders (9.5; 95% CI: 9 to 9.9), non-Hispanic American Indian or Alaska Native (7.8; 95% CI: 6.6 to 9), and Hispanic populations (5.2; 95% CI 5 to 5.5). In addition, non-metropolitan areas had higher AAMRs than metropolitan areas (non-metropolitan areas: 11; 95% CI: 10.8 to 11.2; vs. metropolitan: 9.8; 95% CI: 9.7 to 9.9) (Figure 1).
Conclusions
This analysis revealed a significant decline in mortality since 1999 from TAA, with a slight upward trend in recent years. However, disparities persist, with higher AAMRs observed among men, non-Hispanic African Americans, and residents of non-metropolitan areas.
More abstracts on this topic:
A Comparative Study Of Social Determinants, Hypertension, And Life Essential Factors In Alabama And Colorado From The 2021 Behavioral Risk Factor Surveillance System
Chukwunyere Chibuike, Owuor Kevin
25-Year Decline in Aortic Aneurysm and Dissection Mortality in the U.S.: Impact of Endovascular Repair and Forecast to 2030Ali Manzer, Umar Haddaya, Nazir Tahira, Nizam Muhammad, Steafo Lark, Sharif Ayesha, Jehangir Hanzala, Arham Muhammad, Hamza Anfal, Hassan Arbaz, Amjad Ans, Ali Iman, Zuha Zuha