Final ID: MDP268
Title: Comorbidities Associated with One Year Mortality and Hospital Readmission After Leadless Pacemaker Implantation
Abstract Body (Do not enter title and authors here): Introduction:
Previous studies have noted racial and ethnic disparities in access to leadless pacemaker implantation (LPI), but none have evaluated the socioeconomic disadvantaged (SED). Additionally, few studies have evaluated outcomes of LPI beyond thirty days on a large scale. This study aimed to determine which comorbidities are associated with one-year readmissions and mortality after LPI, including SED via the Social Deprivation Index (SDI).
Methods:
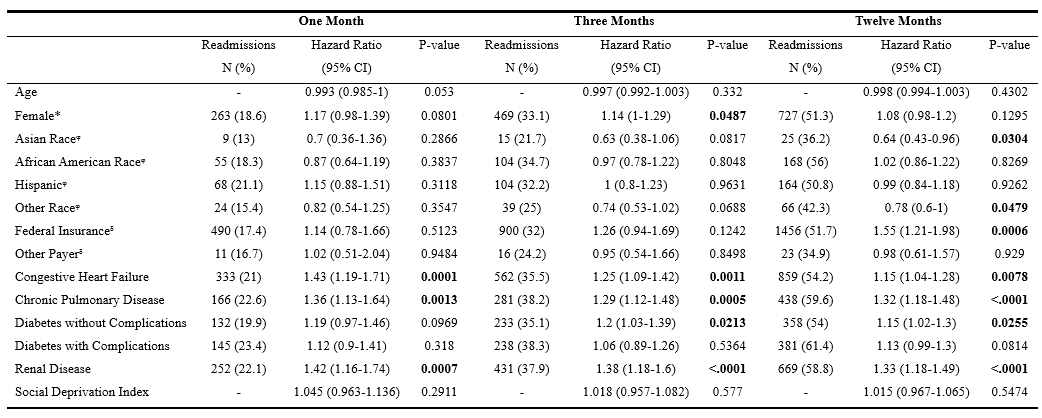
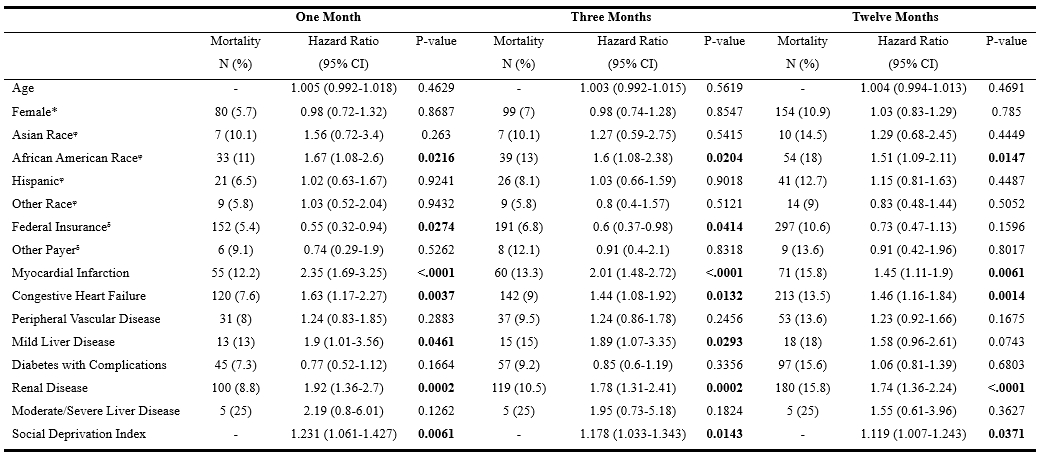
Patients ages ≥18 were identified in the Healthcare Cost and Utilization Project State Inpatient Databases in New York and Florida from 2016-2019 with follow-up into 2020. These states were chosen due to availability for linkage of the 2018 SDI (1-100, higher scores representing more disadvantage). International Classification of Diseases 10 codes for LPI were used. The risk of readmission and mortality was assessed using Cox proportional hazards first in an unadjusted fashion for each comorbidity in the Charlson Comorbidity Index. In addition to demographic variables, only significant variables from the unadjusted analysis were included in the final adjusted multivariable models.
Results:
3,094 patients met inclusion criteria. The readmission and mortality rates at one, three, and twelve months were 17.2%, 31.3%, 50.2% and 5.7%, 7.1%, 10.7%, respectively. The most common diagnoses for readmission were dyspnea/chest pain (9.4%), heart failure (4%), and sepsis (3.8%). Federal insurance, heart failure (CHF), pulmonary disease, diabetes without complications, and renal disease (CKD) were associated with increased risk for twelve-month readmissions. African American race, myocardial infarction, CHF, CKD, and higher SDI were associated with increased risk for twelve-month mortality.
Conclusion:
CHF and CKD put patients at high risk of readmission and mortality. Sepsis was among the most common causes of readmission at twelve months. Patients of higher SED are at increased risk of mortality within one year after LPI.
Previous studies have noted racial and ethnic disparities in access to leadless pacemaker implantation (LPI), but none have evaluated the socioeconomic disadvantaged (SED). Additionally, few studies have evaluated outcomes of LPI beyond thirty days on a large scale. This study aimed to determine which comorbidities are associated with one-year readmissions and mortality after LPI, including SED via the Social Deprivation Index (SDI).
Methods:
Patients ages ≥18 were identified in the Healthcare Cost and Utilization Project State Inpatient Databases in New York and Florida from 2016-2019 with follow-up into 2020. These states were chosen due to availability for linkage of the 2018 SDI (1-100, higher scores representing more disadvantage). International Classification of Diseases 10 codes for LPI were used. The risk of readmission and mortality was assessed using Cox proportional hazards first in an unadjusted fashion for each comorbidity in the Charlson Comorbidity Index. In addition to demographic variables, only significant variables from the unadjusted analysis were included in the final adjusted multivariable models.
Results:
3,094 patients met inclusion criteria. The readmission and mortality rates at one, three, and twelve months were 17.2%, 31.3%, 50.2% and 5.7%, 7.1%, 10.7%, respectively. The most common diagnoses for readmission were dyspnea/chest pain (9.4%), heart failure (4%), and sepsis (3.8%). Federal insurance, heart failure (CHF), pulmonary disease, diabetes without complications, and renal disease (CKD) were associated with increased risk for twelve-month readmissions. African American race, myocardial infarction, CHF, CKD, and higher SDI were associated with increased risk for twelve-month mortality.
Conclusion:
CHF and CKD put patients at high risk of readmission and mortality. Sepsis was among the most common causes of readmission at twelve months. Patients of higher SED are at increased risk of mortality within one year after LPI.
More abstracts on this topic:
Comparative Study of Electrophysiologic Pacing Parameters in Patients with Chagas Disease from Honduras
Baez Andrew, Chavez Dorys, Tracy Cynthia, Mercader Marco
A machine learning model for individualized risk prediction of ischemic heart disease in people with hypertension in ThailandSakboonyarat Boonsub, Poovieng Jaturon, Rangsin Ram