Final ID: Su3182
Socioeconomic Deprivation is Associated with Readmission Within One Year After Atrial Fibrillation Ablation
Abstract Body (Do not enter title and authors here): Introduction:
Gender and race have been shown to impact access and outcomes regarding rhythm control management such as atrial fibrillation (AF) ablation. We aimed to evaluate the role of the Area Deprivation Index (ADI), a validated metric that represents the social disadvantage of communities, to determine if socioeconomic disadvantage (SED) increases the risk of readmission within one year after AF ablation.
Methods:
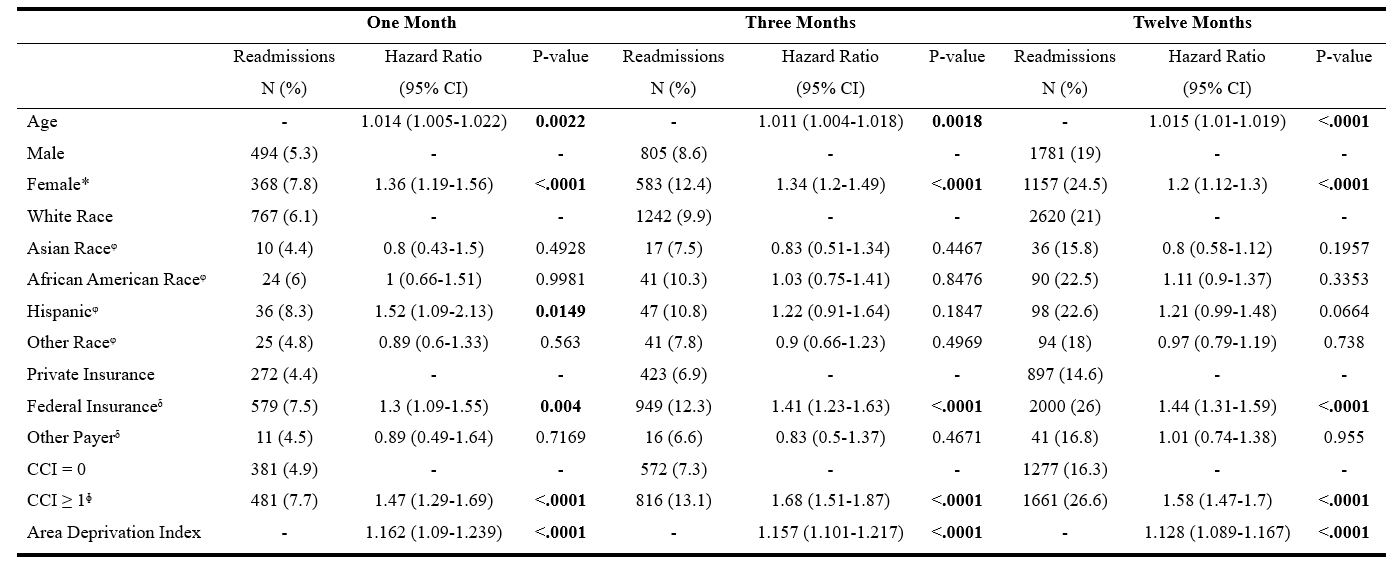
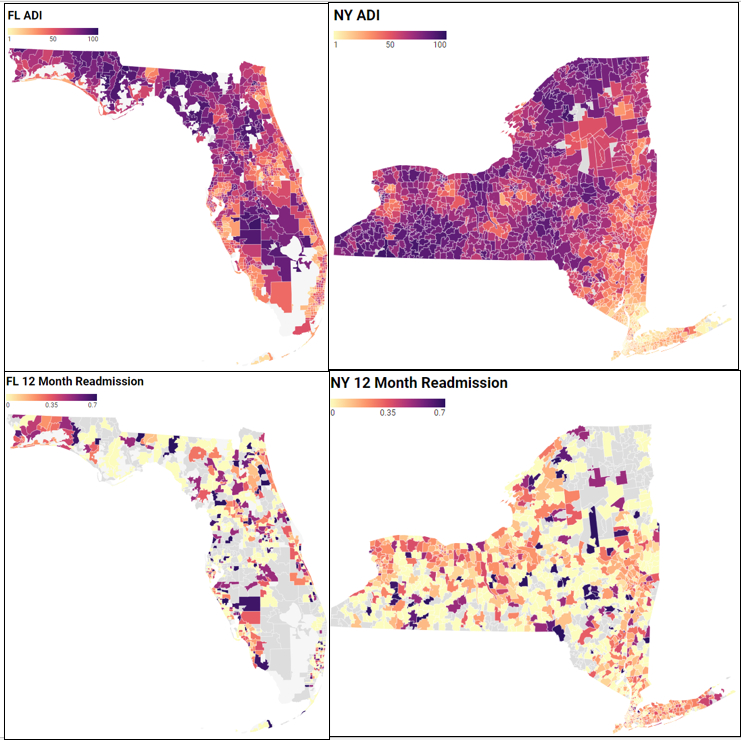
Patients ages ≥18 were identified in the Healthcare Cost and Utilization Project State Ambulatory Surgery and Services Databases in New York and Florida from 2016-2019 with follow-up into 2020 into the inpatient setting. These states were chosen due to availability for linkage of the 2020 ADI. International Classification of Diseases 10 and Current Procedural Terminology codes for AF and AF ablation were used. The risk of readmission was assessed using multivariable Cox proportional hazards with covariates age, sex, race, insurance, Charlson Comorbidity Index (0 vs ≥ 1 comorbidity), and ADI quartiles. ADI is scored 1-100 with higher scores representing more disadvantage.
Results:
14,078 patients met inclusion criteria. The readmission rate at one, three, and twelve months was 6.1%, 9.9%, and 20.9% respectively. The most common readmission diagnoses at twelve months were AF (22.8%), followed by symptoms such as chest pain, dyspnea, palpitations, and syncope (13%). In the adjusted model, older age, female sex, federal insurance, ≥ 1 Charlson comorbidity, and higher ADI had higher one-, three-, and twelve-month risks of readmission. Hispanic ethnicity had a higher risk of one month readmission.
Conclusion:
Readmission for AF after ablation is common at twelve months. Higher risk of readmission after AF ablation was observed with SED. Enhanced awareness and additional research regarding SED as a risk factor for readmission may help improve post-ablation AF outcomes and equitable access to cardiovascular care.
Gender and race have been shown to impact access and outcomes regarding rhythm control management such as atrial fibrillation (AF) ablation. We aimed to evaluate the role of the Area Deprivation Index (ADI), a validated metric that represents the social disadvantage of communities, to determine if socioeconomic disadvantage (SED) increases the risk of readmission within one year after AF ablation.
Methods:
Patients ages ≥18 were identified in the Healthcare Cost and Utilization Project State Ambulatory Surgery and Services Databases in New York and Florida from 2016-2019 with follow-up into 2020 into the inpatient setting. These states were chosen due to availability for linkage of the 2020 ADI. International Classification of Diseases 10 and Current Procedural Terminology codes for AF and AF ablation were used. The risk of readmission was assessed using multivariable Cox proportional hazards with covariates age, sex, race, insurance, Charlson Comorbidity Index (0 vs ≥ 1 comorbidity), and ADI quartiles. ADI is scored 1-100 with higher scores representing more disadvantage.
Results:
14,078 patients met inclusion criteria. The readmission rate at one, three, and twelve months was 6.1%, 9.9%, and 20.9% respectively. The most common readmission diagnoses at twelve months were AF (22.8%), followed by symptoms such as chest pain, dyspnea, palpitations, and syncope (13%). In the adjusted model, older age, female sex, federal insurance, ≥ 1 Charlson comorbidity, and higher ADI had higher one-, three-, and twelve-month risks of readmission. Hispanic ethnicity had a higher risk of one month readmission.
Conclusion:
Readmission for AF after ablation is common at twelve months. Higher risk of readmission after AF ablation was observed with SED. Enhanced awareness and additional research regarding SED as a risk factor for readmission may help improve post-ablation AF outcomes and equitable access to cardiovascular care.
More abstracts on this topic:
Association of Childhood Opportunity Index and No Show Rates in a Pediatric Cardiology Clinic.
Elliott Pietro, Ather Mishaal, Lynch Miranda, Guglielmo Kimberly, Chowdhury Devyani
A Potential Role for NKG2D, an NK cell receptor, in Accelerated CVD risk in African American Women Living in More Adverse Neighborhood Conditions: Data From the Step It Up Physical Activity Digital Health-Enabled, Community-Engaged InterventionBaez Andrew, Andrews Marcus, Sandler Dana, Aquino Peterson Elizabeth, Sharda Sonal, Tolentino Katherine Joy, Lopez De Leon Shirley, Seo Jein Eleanor, Cintron Manuel, Pita Mario, Tarfa Hannatu, Baumer Yvonne, Reger Robert, Childs Richard, Powell-wiley Tiffany, Dave Ayushi, Saurabh Abhinav, Mendelsohnl Laurel, Chen Long, Igboko Muna, Wells Ayanna, Marah Marie