Final ID: MDP1239
Persistent Disparities in Chronic Ischemic Heart Disease-Related Mortality across Age, Sex, Race/Ethnicity in the United States, 1999 - 2020
Abstract Body (Do not enter title and authors here): BACKGROUND
Chronic Ischemic Heart Disease (CIHD) is a heterogeneous group of cardiac diseases that cause significant morbidity and mortality. Previous studies demonstrated a decline in CIHD mortality rate (MR) but there is paucity of data on contemporary trends across different demographics in the United States (US). We examined the national trends in age-adjusted CIHD-MR (overall and stratified by demographics) in the US from 1999 to 2020.
METHODS
We retrospectively analyzed national death certificate data from the CDC WONDER database from 1999 to 2020. The underlying cause of death from CIHD was identified with ICD-10 code I25 in adults aged ≥35 years and the age-adjusted mortality rate was calculated per 100,000 population. We categorized race/ethnicity as Non-Hispanic White (NHW), Non-Hispanic Black (NHB), Latino or Hispanic, and other non-Hispanic groups. Trends in age-adjusted CIHD-MR (AAMR) were analyzed by age, gender, race/ethnicity, and geographic region were evaluated with Joinpoint regression, and expressed as an average annual percentage change (AAPC) with a 95% confidence interval. For sensitivity analysis, we repeated the study with data from death certificates that had CIHD as a contributing cause of death.
RESULTS
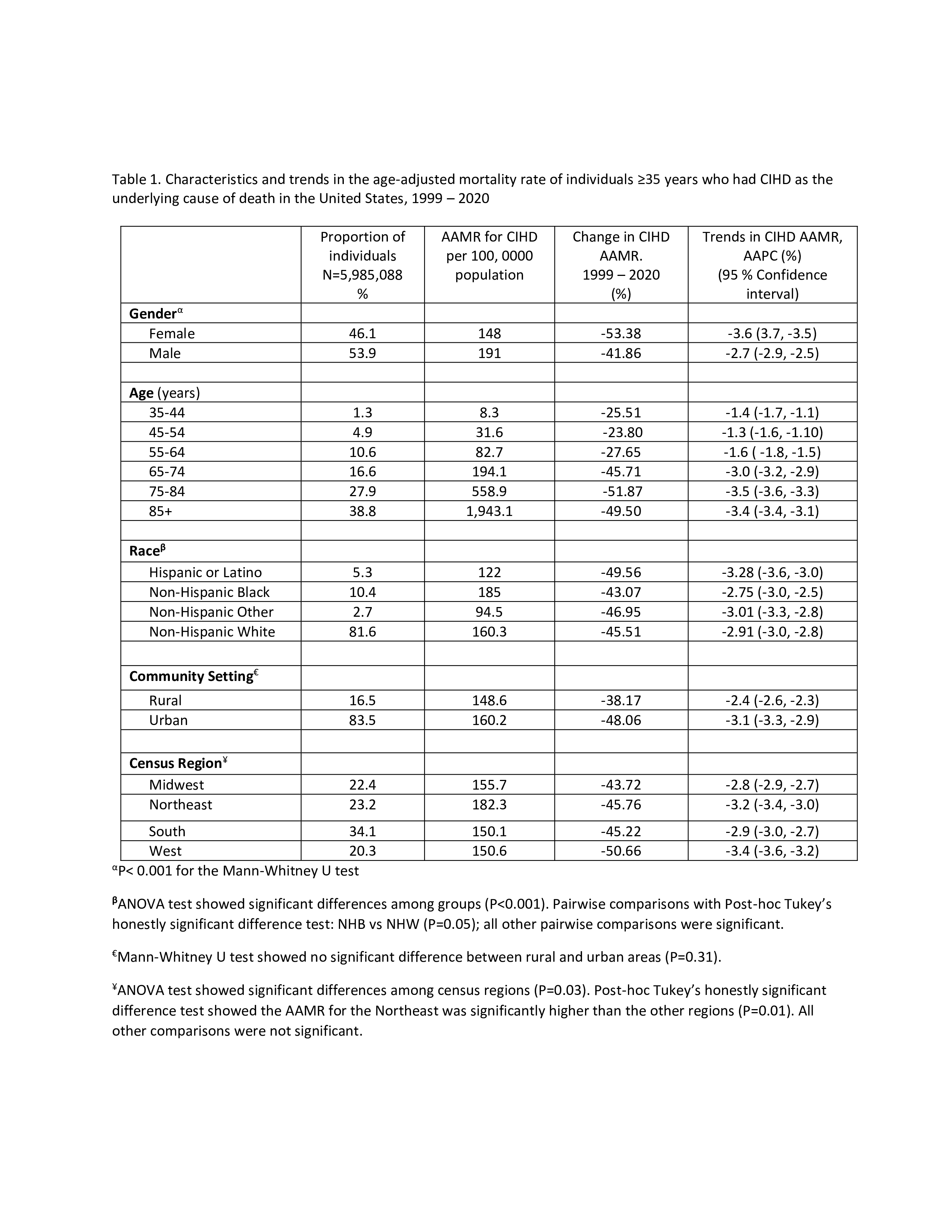
Out of 3.55 billion people aged ≥ 35 years, 5,985,088 died of CIHD (AAMR: 158.2 per 100, 000) [53.9% male, 81.6% NHW, 38.8% ≥85 years]. The AAMR was highest in males, the Northeast region, and NHB (Table 1). The AAMR was highest in those aged ≥85 years and was directly related to age (35-44 years: 8.3 per 100,000; ≥85 years: 1,943 per 100,000). The CIHD AAMR declined significantly overall in males, all races/ethnicities, and geographical areas (Table 1). Reanalysis (Sensitivity analysis) with any mention of CIHD as a contributing cause of death showed similar trends.
CONCLUSION
Over the 22 years, CIHD-related mortality in the US has declined overall and for almost all demographic groups. However, there are age, gender, and racial disparities in the CIHD AAMR. These findings highlight the need for further longitudinal studies to understand the drivers of these disparities and for focused public health interventions to improve CIHD mortality outcomes in these populations.
Chronic Ischemic Heart Disease (CIHD) is a heterogeneous group of cardiac diseases that cause significant morbidity and mortality. Previous studies demonstrated a decline in CIHD mortality rate (MR) but there is paucity of data on contemporary trends across different demographics in the United States (US). We examined the national trends in age-adjusted CIHD-MR (overall and stratified by demographics) in the US from 1999 to 2020.
METHODS
We retrospectively analyzed national death certificate data from the CDC WONDER database from 1999 to 2020. The underlying cause of death from CIHD was identified with ICD-10 code I25 in adults aged ≥35 years and the age-adjusted mortality rate was calculated per 100,000 population. We categorized race/ethnicity as Non-Hispanic White (NHW), Non-Hispanic Black (NHB), Latino or Hispanic, and other non-Hispanic groups. Trends in age-adjusted CIHD-MR (AAMR) were analyzed by age, gender, race/ethnicity, and geographic region were evaluated with Joinpoint regression, and expressed as an average annual percentage change (AAPC) with a 95% confidence interval. For sensitivity analysis, we repeated the study with data from death certificates that had CIHD as a contributing cause of death.
RESULTS
Out of 3.55 billion people aged ≥ 35 years, 5,985,088 died of CIHD (AAMR: 158.2 per 100, 000) [53.9% male, 81.6% NHW, 38.8% ≥85 years]. The AAMR was highest in males, the Northeast region, and NHB (Table 1). The AAMR was highest in those aged ≥85 years and was directly related to age (35-44 years: 8.3 per 100,000; ≥85 years: 1,943 per 100,000). The CIHD AAMR declined significantly overall in males, all races/ethnicities, and geographical areas (Table 1). Reanalysis (Sensitivity analysis) with any mention of CIHD as a contributing cause of death showed similar trends.
CONCLUSION
Over the 22 years, CIHD-related mortality in the US has declined overall and for almost all demographic groups. However, there are age, gender, and racial disparities in the CIHD AAMR. These findings highlight the need for further longitudinal studies to understand the drivers of these disparities and for focused public health interventions to improve CIHD mortality outcomes in these populations.
More abstracts on this topic:
A machine learning model for individualized risk prediction of ischemic heart disease in people with hypertension in Thailand
Sakboonyarat Boonsub, Poovieng Jaturon, Rangsin Ram
Anomalous Origins: Hereditary Transthyretin Cardiac Amyloidosis Mimicking Ischemia in a Patient with Congenital Coronary AnomaliesLabin Jonathan, Carmona Rubio Andres, Liu Joseph, Hanna Mazen, Menon Venu, Higgins Andrew