Final ID: Su2171
Hemodynamic Indices of Right Ventricular Function Differentially Predict Adverse Clinical Outcomes in Heart Failure with Preserved vs Reduced Ejection Fraction
Abstract Body (Do not enter title and authors here):
Background: While the critical role of right ventricular dysfunction (RVD) in heart failure (HF) is increasingly recognized, the prevalence and prognostic impact of RVD across HF subtypes is poorly understood.
Research Questions/Aims: We aimed to characterize differences in hemodynamic indices of RV function among patients with HF with preserved vs reduced ejection fraction (HFpEF, EF≥50% vs HFrEF, EF<50%) and to examine associations of RVD with longitudinal clinical outcomes by HF subtype.
Methods: We identified patients with prevalent HF undergoing clinically indicated right heart catheterization at Massachusetts General Hospital (2005-2016). We examined three RV hemodynamic indices: right atrial to wedge pressure ratio (RA/PCWP), RV stroke work index (RVSWI), and pulmonary artery pulsatility index (PAPi). We used multivariable linear regression to assess differences in RV indices in HFpEF vs HFrEF. We then used Cox models to examine the association of each index with HF hospitalizations (HFH), major adverse cardiac events (MACE), and death, stratified by HF subtype. Models were adjusted for age, sex, BMI, hypertension, diabetes, lung disease, sleep apnea, and prior MI.
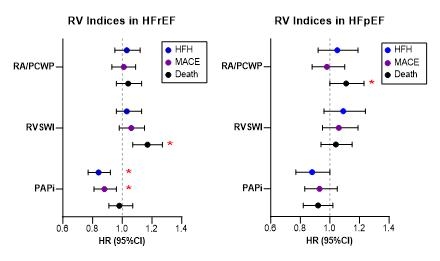
Results: Of 2,062 patients (age 66 years, 33% women), 1,242 (60%) had HFrEF and 820 (40%) had HFpEF. RVD (RVSWI <450 mm Hg*ml/m2) was present in 27% of HFrEF vs 21% of HFpEF patients. Those with HFpEF had higher RA/PCWP (β 0.12, SE 0.05, p=0.012) and RVSWI (β 0.22, SE 0.05, p<0.001) relative to HFrEF. Over 4.1 median years follow-up, 915 HFH, 1,066 MACE, and 1,116 death events occurred. Among those with HFrEF, lower PAPi was associated with greater risk of HFH (HR 0.84 (0.77, 0.92); p<0.001) and MACE (HR 0.88 (0.81, 0.96); p=0.003), and higher RVSWI was associated with greater risk of death (HR 1.17, (1.07, 1.27); p<0.001, Figure). In contrast, in those with HFpEF, only higher RA/PCWP was associated with greater risk of death (HR 1.11 (1.00, 1.23); p=0.042).
Conclusion: RVD occurs frequently in both HFrEF and HFpEF, and hemodynamic measures of RV function are associated with greater risk of MACE, death, and HFH. Importantly, the prognostic value of RV indices varied by HF subtype, highlighting key differences in the role of RVD in HFrEF vs HFpEF.
Background: While the critical role of right ventricular dysfunction (RVD) in heart failure (HF) is increasingly recognized, the prevalence and prognostic impact of RVD across HF subtypes is poorly understood.
Research Questions/Aims: We aimed to characterize differences in hemodynamic indices of RV function among patients with HF with preserved vs reduced ejection fraction (HFpEF, EF≥50% vs HFrEF, EF<50%) and to examine associations of RVD with longitudinal clinical outcomes by HF subtype.
Methods: We identified patients with prevalent HF undergoing clinically indicated right heart catheterization at Massachusetts General Hospital (2005-2016). We examined three RV hemodynamic indices: right atrial to wedge pressure ratio (RA/PCWP), RV stroke work index (RVSWI), and pulmonary artery pulsatility index (PAPi). We used multivariable linear regression to assess differences in RV indices in HFpEF vs HFrEF. We then used Cox models to examine the association of each index with HF hospitalizations (HFH), major adverse cardiac events (MACE), and death, stratified by HF subtype. Models were adjusted for age, sex, BMI, hypertension, diabetes, lung disease, sleep apnea, and prior MI.
Results: Of 2,062 patients (age 66 years, 33% women), 1,242 (60%) had HFrEF and 820 (40%) had HFpEF. RVD (RVSWI <450 mm Hg*ml/m2) was present in 27% of HFrEF vs 21% of HFpEF patients. Those with HFpEF had higher RA/PCWP (β 0.12, SE 0.05, p=0.012) and RVSWI (β 0.22, SE 0.05, p<0.001) relative to HFrEF. Over 4.1 median years follow-up, 915 HFH, 1,066 MACE, and 1,116 death events occurred. Among those with HFrEF, lower PAPi was associated with greater risk of HFH (HR 0.84 (0.77, 0.92); p<0.001) and MACE (HR 0.88 (0.81, 0.96); p=0.003), and higher RVSWI was associated with greater risk of death (HR 1.17, (1.07, 1.27); p<0.001, Figure). In contrast, in those with HFpEF, only higher RA/PCWP was associated with greater risk of death (HR 1.11 (1.00, 1.23); p=0.042).
Conclusion: RVD occurs frequently in both HFrEF and HFpEF, and hemodynamic measures of RV function are associated with greater risk of MACE, death, and HFH. Importantly, the prognostic value of RV indices varied by HF subtype, highlighting key differences in the role of RVD in HFrEF vs HFpEF.
More abstracts on this topic:
Association Between Genetics Variants And Clinical Outcomes In Patients With Left Ventricular Assist Device
Silver Elizabeth, Hong Kimberly, Tran Hao, Pretorius Victor, Kearns Mark, Urey Marcus, Adler Eric, Bui Quan
Abnormal day-night blood pressure and systemic hemodynamics in heart failure compared to normotension and controlled hypertensionSrungavarapu Sambasiva Rao, Khatri Chander, Osmond Peter, Izzo Joseph