Final ID: MDP516
Monosialoganglioside-containing nanoliposomes protect against acute and chronic ischemic stroke injury
Abstract Body (Do not enter title and authors here): BACKGROUND: Stroke remains a leading cause of mortality and disability. The narrow temporal window and limited availability of, and eligibility for thrombolytic therapy or endovascular thrombectomy are major therapeutic limitations in treating stroke. Neuroprotective therapies that could be given early to replace or augment these existing therapies are needed to improve stroke outcomes. We showed that monosialoganglioside (GM1) containing nanoliposomes composed of phosphatidylcholine, cholesterol and GM1 (70/25/5% molar ratios, NLGM1) protect against hypoxic injury likely through Nrf2-dependent upregulation of antoxidant enzymes.
AIMS: To test if post-occlusion NLGM1 treatment could reduce 1) acute stroke injury following middle cerebral artery occlusion (MCAO) and 2) chronic injury following photothrombotic (PT) stroke injury.
METHODS: 20 week old C57BL/6 mice underwent MCAO for 60 minutes and then injected with saline or NLGM1 (1 or 2 mg IV) prior to reperfusion. Neurologic deficit score and brain infarct % area were measured the next day. Separately, mice underwent PT injury followed by injection of saline or NLGM1 (1 or 2 mg immediately and 2 hours post-injury) and cognitive/behavior tests done 1-90 days post injury.
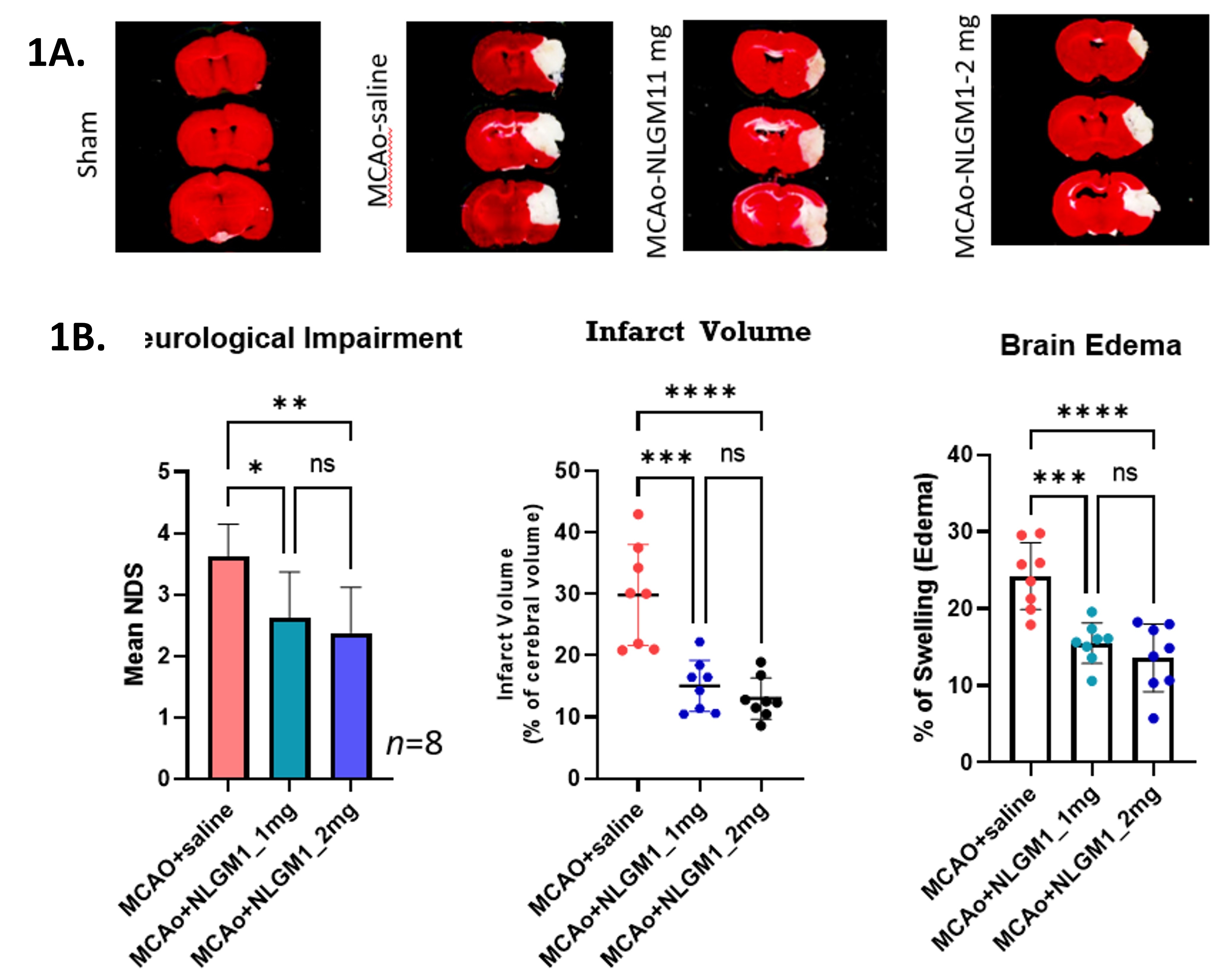
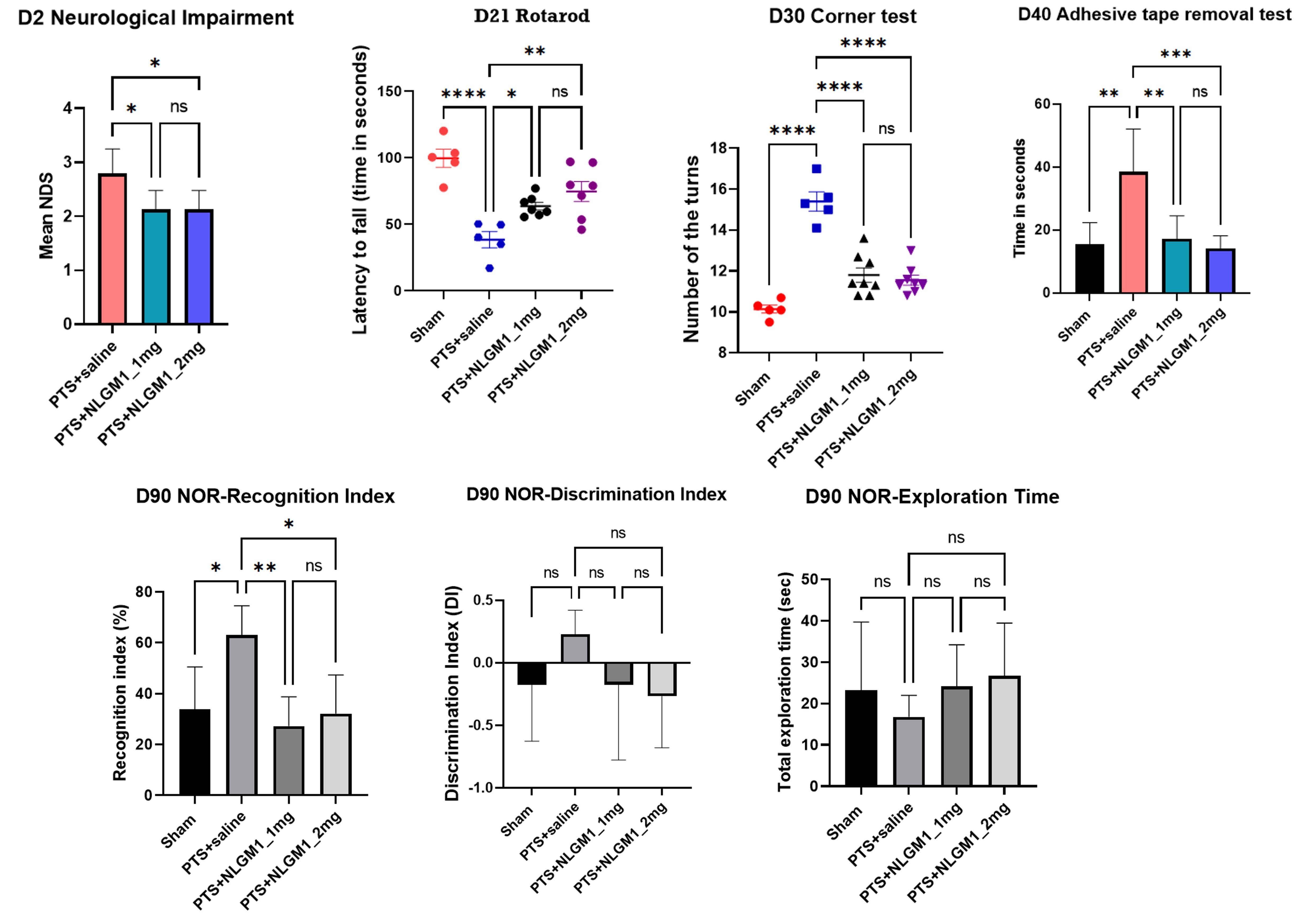
RESULTS: Following MCAO, there was reduced neurologic impairment, infarct volume and brain edema with NLGM1 versus saline control (Fig. 1). Following PT injury, there was reduced neurologic, cognitive and motor impairment from Day 2-90 post-injury with NLGM1 versus saline control (Fig. 2). In both stroke models, there was no difference in efficacy between 1 and 2 mg NLGM1 doses.
CONCLUSIONS: Treatment of mice with NLGM1 following MCAO or PT stroke injury resulted in improved structural (infarct size, edema) and functional (cognitive, behavior, motor) outcomes in the acute (MCAO) and chronic (PT) timeframes. NLGM1 is a potential novel therapeutic agent for stroke.
AIMS: To test if post-occlusion NLGM1 treatment could reduce 1) acute stroke injury following middle cerebral artery occlusion (MCAO) and 2) chronic injury following photothrombotic (PT) stroke injury.
METHODS: 20 week old C57BL/6 mice underwent MCAO for 60 minutes and then injected with saline or NLGM1 (1 or 2 mg IV) prior to reperfusion. Neurologic deficit score and brain infarct % area were measured the next day. Separately, mice underwent PT injury followed by injection of saline or NLGM1 (1 or 2 mg immediately and 2 hours post-injury) and cognitive/behavior tests done 1-90 days post injury.
RESULTS: Following MCAO, there was reduced neurologic impairment, infarct volume and brain edema with NLGM1 versus saline control (Fig. 1). Following PT injury, there was reduced neurologic, cognitive and motor impairment from Day 2-90 post-injury with NLGM1 versus saline control (Fig. 2). In both stroke models, there was no difference in efficacy between 1 and 2 mg NLGM1 doses.
CONCLUSIONS: Treatment of mice with NLGM1 following MCAO or PT stroke injury resulted in improved structural (infarct size, edema) and functional (cognitive, behavior, motor) outcomes in the acute (MCAO) and chronic (PT) timeframes. NLGM1 is a potential novel therapeutic agent for stroke.
More abstracts on this topic:
A Phase 2 Study Evaluating the Effects of Mivelsiran, an Investigational RNA Interference Therapeutic, on Hemorrhagic and Nonhemorrhagic Manifestations of Cerebral Amyloid Angiopathy
Greenberg Steven, Parikh Neal, Lee Jin-moo, Van Etten Ellis, Van Osch Matthias, Klijn Catharina, Sostelly Alexandre, Goteti Sasikiran, Sepehrband Farshid, Avbersek Andreja, Deering Robert
A distinct clot transcriptomic signature is associated with atrial fibrillation-derived ischemic stroke in the INSIGHT RegistrySeah Carina, Rivet Dennis, Fraser Justin, Kellner Christopher, Devarajan Alex, Vicari James, Dabney Alan, Baltan Selva, Sohrabji Farida, Pennypacker Keith, Nanda Ashish, Woodward Britton