Final ID: Sa4042
Risk Factors Associated with Cardiac Hospital Admissions in Cancer Patients Treated with Immune Checkpoint Inhibitors
Abstract Body (Do not enter title and authors here): Background: Immune checkpoint inhibitors (ICIs) are highly effective anti-cancer treatments for several cancers. However, treatment with ICIs is associated with metabolic perturbations, accelerated atherosclerosis, and increased risks of adverse cardiovascular events. In this study, we aimed to determine risk factors associated with cardiac hospital admissions in patients treated with ICIs for their cancer.
Methods: Retrospective data was collected for all patients treated with ICIs between 1 January 2010 and 1 January 2020 through the Hunter New England Local Health District (HNELHD), Australia. Patient medical history and demographics were collected through electronic medical records. Outcome data was obtained from the HNELHD Institutional Cardiac and Stroke Outcomes Unit database. Cardiac admission was defined as cardiac disease based on hospital administration ICD-10 codes. Binary logistic regression was used for multivariate analysis and performed through SPSS version 28.
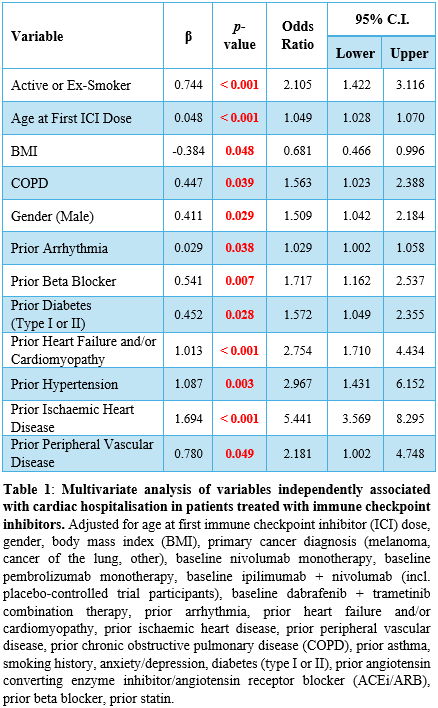
Results: A total of 1,080 patients were included in the final analysis. Mean age of patients was 66.9 ± 11.7 years, with the majority male sex (n=685; 63.4%). Primary cancer diagnosis of patients treated with ICIs included melanoma (n=417; 38.7%), and cancer of the lung (n=327; 30.3%). Nivolumab monotherapy was the most used first-line ICI treatment (n=475; 44.0%) followed by pembrolizumab monotherapy (n=428; 39.6%). A total of 266 (24.6%) patients had at least one cardiac hospital admission. On univariate analysis, pre-existing cardiovascular disease (CVD) (p<0.001), diabetes mellitus (p<0.001), chronic kidney disease (p<0.001), and prior CVD medications (p<0.001) were associated with cardiac hospitalisation. On multivariate analysis, prior history of heart failure (p<0.001), hypertension (p=0.003), ischaemia, and peripheral vascular disease (p=0.049) were independently associated with an increased risk of cardiac hospital admission.
Conclusions: In cancer patients treated with ICIs, pre-existing CVD risk factors increases the risk of cardiac-associated hospitalisations. Adequate CVD risk modification and monitoring during treatment with ICIs may be necessary to reduce cardiac hospitalisations.
Methods: Retrospective data was collected for all patients treated with ICIs between 1 January 2010 and 1 January 2020 through the Hunter New England Local Health District (HNELHD), Australia. Patient medical history and demographics were collected through electronic medical records. Outcome data was obtained from the HNELHD Institutional Cardiac and Stroke Outcomes Unit database. Cardiac admission was defined as cardiac disease based on hospital administration ICD-10 codes. Binary logistic regression was used for multivariate analysis and performed through SPSS version 28.
Results: A total of 1,080 patients were included in the final analysis. Mean age of patients was 66.9 ± 11.7 years, with the majority male sex (n=685; 63.4%). Primary cancer diagnosis of patients treated with ICIs included melanoma (n=417; 38.7%), and cancer of the lung (n=327; 30.3%). Nivolumab monotherapy was the most used first-line ICI treatment (n=475; 44.0%) followed by pembrolizumab monotherapy (n=428; 39.6%). A total of 266 (24.6%) patients had at least one cardiac hospital admission. On univariate analysis, pre-existing cardiovascular disease (CVD) (p<0.001), diabetes mellitus (p<0.001), chronic kidney disease (p<0.001), and prior CVD medications (p<0.001) were associated with cardiac hospitalisation. On multivariate analysis, prior history of heart failure (p<0.001), hypertension (p=0.003), ischaemia, and peripheral vascular disease (p=0.049) were independently associated with an increased risk of cardiac hospital admission.
Conclusions: In cancer patients treated with ICIs, pre-existing CVD risk factors increases the risk of cardiac-associated hospitalisations. Adequate CVD risk modification and monitoring during treatment with ICIs may be necessary to reduce cardiac hospitalisations.
More abstracts on this topic:
A Machine Learning Readmission Risk Prediction Model for Cardiac Disease
Bailey Angela, Wang Wei, Shannon Clarence, Huling Jared, Tignanelli Christopher
Association Between In-hospital Cardiac Arrest Incidence and Survival in Older PatientsNathani Rohit, Li Qiang, Nguyen Cathy, Koshy Thomas, Hall Hurst, Mentias Amgad, Chan Paul, Girotra Saket