Final ID: MDP402
Higher Global Registry of Acute Coronary Events Score is Associated with Lower Invasive Coronary Angiograpy Use
Abstract Body (Do not enter title and authors here): Background: Use of invasive coronary angiography (ICA) and the selection of other interventions in patients who present with NSTEMI should be guided by clinical risk stratification. National guidelines recommend ICA use in patients with intermediate and high risk scores. The Global Registry of Acute Coronary Events (GRACE) score is a commonly used risk score that is based on clinical characteristics available at the time of admission.
Aim: Examine if patients with NSTEMI with higher risk stratification scores are more likely to have ICA.
Methods: This cross-sectional study included all patients who presented with NSTEMI to an academic medical center that serves a rural population over a 12-month period. Data were derived from the American College of Cardiology Chest Pain – MI Registry data collected by trained abstractors at the facility and were verifed by the study team. Additional data needed to calculate the GRACE Score were abstracted by the study team. GRACE Scores were categorized into low (1-88), moderate (89-118), and high (119-263) risk. Multivariable logistic regression was used to test if higher GRACE scores are more associated with ICA use controlling for patient factors not included in the GRACE Score and further examined by GRACE score category.
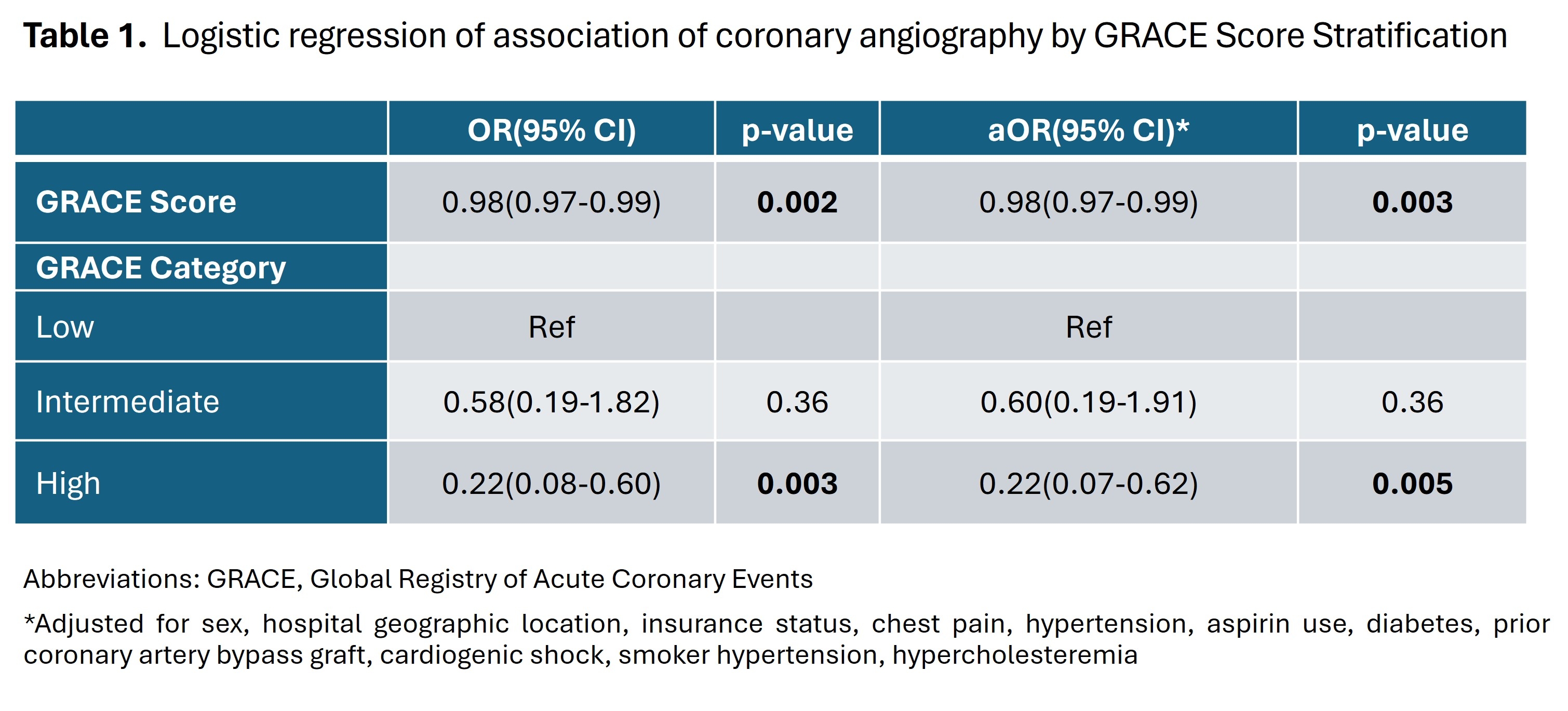
Results: The total sample size was 434 patients (Mean age 65±13.8, 36% female and 36% Black). Patients transferred from outlying facilities accounted for 40% of the sample. ICA was performed for 94% of the patients. Increasing GRACE score was associated with lower ICA use (aOR 0.98, 95% CI 0.97-0.99). Odds of ICA use between the low-risk group and the intermediate risk group (aOR 0.60, 95% CI 0.19-1.91) did not significantly differ. Patients in the high-risk category were less likely to undergo ICA compated to low-risk patients (aOR 0.22, 95% CI 0.07-0.62).
Conclusions: Use of ICA decreased as GRACE score increased in this patient sample, suggesting that additional factors beyond GRACE score likely influence ICA use in patients who presented with NSTEMI during this time period. Influence of patient factors as well as provider and patient risk aversion on ICA selection must be explored to better understand incongruence with guideline recommendations.
Aim: Examine if patients with NSTEMI with higher risk stratification scores are more likely to have ICA.
Methods: This cross-sectional study included all patients who presented with NSTEMI to an academic medical center that serves a rural population over a 12-month period. Data were derived from the American College of Cardiology Chest Pain – MI Registry data collected by trained abstractors at the facility and were verifed by the study team. Additional data needed to calculate the GRACE Score were abstracted by the study team. GRACE Scores were categorized into low (1-88), moderate (89-118), and high (119-263) risk. Multivariable logistic regression was used to test if higher GRACE scores are more associated with ICA use controlling for patient factors not included in the GRACE Score and further examined by GRACE score category.
Results: The total sample size was 434 patients (Mean age 65±13.8, 36% female and 36% Black). Patients transferred from outlying facilities accounted for 40% of the sample. ICA was performed for 94% of the patients. Increasing GRACE score was associated with lower ICA use (aOR 0.98, 95% CI 0.97-0.99). Odds of ICA use between the low-risk group and the intermediate risk group (aOR 0.60, 95% CI 0.19-1.91) did not significantly differ. Patients in the high-risk category were less likely to undergo ICA compated to low-risk patients (aOR 0.22, 95% CI 0.07-0.62).
Conclusions: Use of ICA decreased as GRACE score increased in this patient sample, suggesting that additional factors beyond GRACE score likely influence ICA use in patients who presented with NSTEMI during this time period. Influence of patient factors as well as provider and patient risk aversion on ICA selection must be explored to better understand incongruence with guideline recommendations.
More abstracts on this topic:
A Rare Case of Sequential Impella Mechanical Failures due to Infective Endocarditis Vegetations
Sawalski Cathryn, Seu Michelle, Darki Amir
A Randomized Clinical Trial Evaluating Vitamin D Normalization on Major Adverse Cardiovascular-Related Events Among Acute Coronary Syndrome Patients: The TARGET-D TrialMay Heidi, Colipi Dominique, Whiting Tyler, Muhlestein Joseph, Le Viet, Anderson Jeffrey, Babcock Daniel, Wayman Libby, Bair Tami, Knight Stacey, Knowlton Kirk, Iverson Leslie