Final ID: Th0078
Peripheral Artery Calcification Disrupts Lower Extremity Biomechanics In a Swine Model
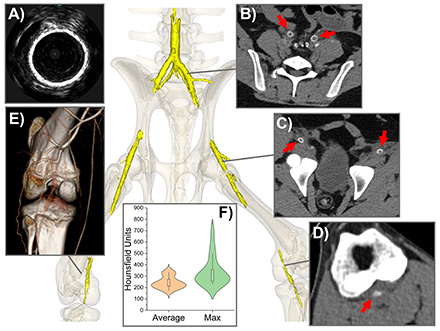
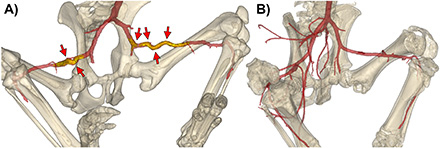
Abstract Body: Limb flexion imposes severe deformations on lower extremity arteries, altering blood flow and contributing to the progression of Peripheral Artery Disease (PAD) and treatment failure. While arterial calcification is associated with poor clinical outcomes and an elevated risk of amputation, its biomechanical effects remain poorly understood. Using a swine model of advanced arterial calcification, we investigated the impact of arterial calcium on limb flexion-induced biomechanics while controlling for confounding variables. Calcification was induced by delivering CaCl2 into the media and periadventitial spaces of the iliac, femoral, and popliteal arteries via a micro-needle catheter. This approach produced robust calcific lesions (Figure 1), clearly visible on computed tomography and intravascular ultrasound within 30 days, and closely mimicking human calcification in morphology, mechanics, and histology. Experimental (n=6) and control (n=27) animals were imaged with their limbs in straight and flexed positions (Figure 2). Reconstructed 3D arterial geometries revealed significant differences in diameters, foreshortening, tortuosity, and angulation between calcified and non-calcified arteries. Calcified arteries exhibited 15% larger diameters (7.1 vs. 6.2 mm, p=0.048) and accommodated 41% less foreshortening during flexion (1.29 vs. 1.49, p<0.01), resulting in increased tortuosity and sharper bends. Tortuosity increased by 61% in the external iliac artery (0.06 vs. 0.04), 49% in the superficial femoral artery (SFA, 0.20 vs 0.13), and 19% in the popliteal artery (PA, 0.36 vs. 0.30) (all p<0.01). Bending severity, assessed via inscribed sphere measurements and angles, was 52% greater at the inguinal ligament (11.4 vs 23.8 mm), 43% greater in the SFA (16.9 vs 29.7 mm), and 59% greater in the PA (5.9 vs 14.1 mm) (all p<0.01) in animals with calcific lesions. This porcine model replicates critical features of calcific human PAD in a rigorously controlled environment, enabling detailed biomechanical analysis. Furthermore, it provides a robust platform to evaluate the impacts and mechanisms of calcium-modifying treatments, offering valuable insights for improving therapeutic strategies. Our findings demonstrate that arterial calcification significantly impairs the ability of arteries to accommodate limb flexion, exacerbates bending and tortuosity, and likely contributes to impaired blood flow, PAD progression, and treatment failure.
More abstracts on this topic:
Albumin for Patients With Acute large Vessel Occlusive Stroke Undergoing Endovascular Treatment: A Multicenter, Randomized Double-blind, Placebo-Controlled Clinical Trail
Ji Xunming, Wu Chuanjie, Li Chuanhui, Liu Yuanyuan, Dong Xiao, Ma Zhengfei, Wu Di, Xu Yi, Zhou Chen
9p21.3 variants drive coronary calcification by suppressing statherin expressionSoheili Fariborz, Almontashiri Naif, Heydarikhorneh Niloufar, Vilmundarson Ragnar, Chen Hsiao-huei, Stewart Alexandre