Final ID: Sa1405
Heart rhythm at hospital admission: a factor for survival and neurological outcome among ECPR recipients?
Abstract Body: Objectives: The initial rhythm is a well-established predictor of survival among extracorporeal cardiopulmonary resuscitation (ECPR) recipients. However, the impact of rhythm at hospital admission on outcomes in ECPR patients is less understood. This study aimed to analyze the relationship between the rhythm at hospital admission and survival, as well as neurological outcomes, among ECPR recipients.
Methods: In this prospective, observational, single-center registry study, the impact of the rhythm at hospital admission (ventricular fibrillation, pulseless electrical activity, or asystole) on 30-day survival and neurological outcomes at discharge was evaluated among patients who received ECPR for out-of-hospital cardiac arrest (OHCA).
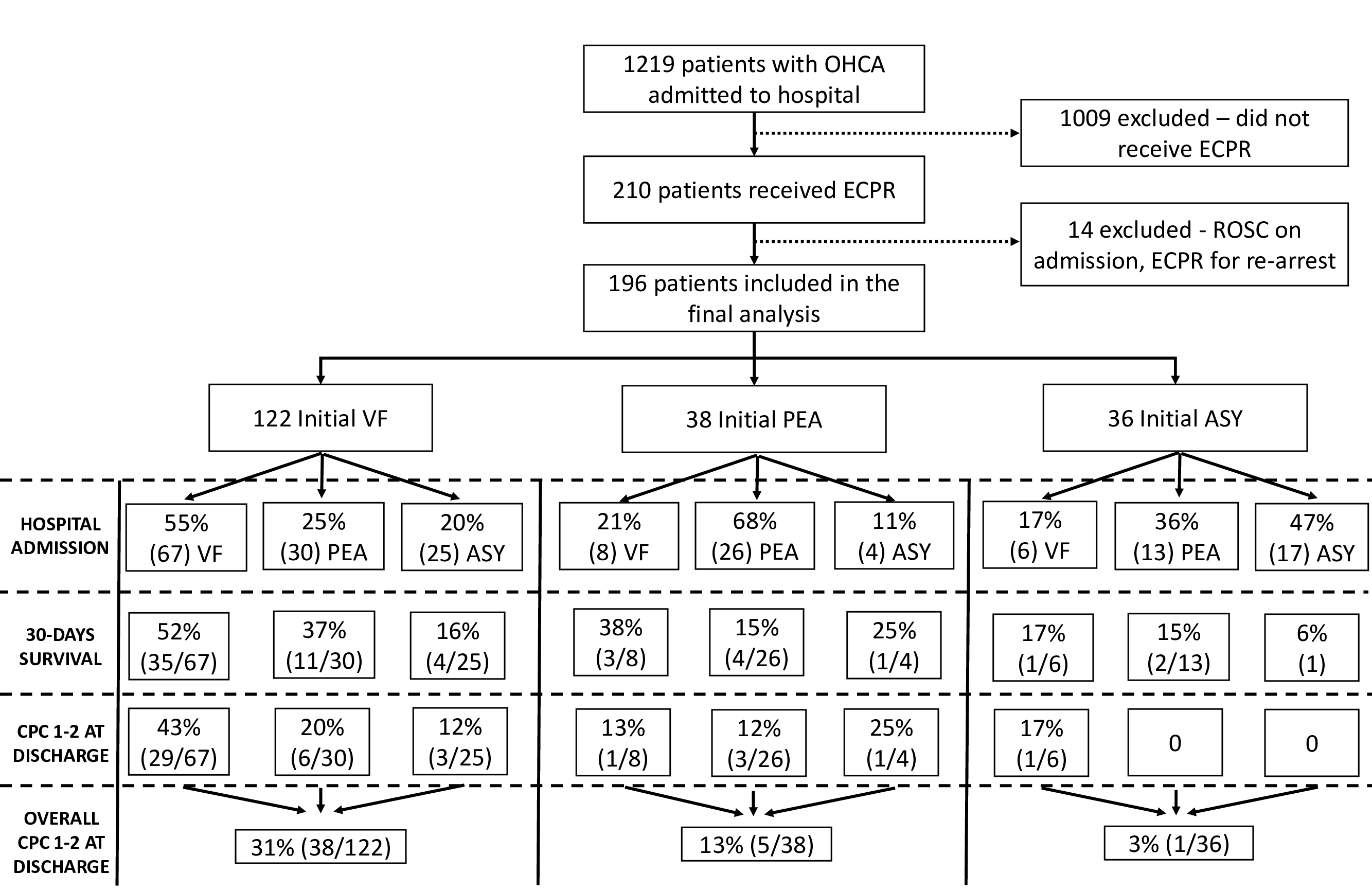
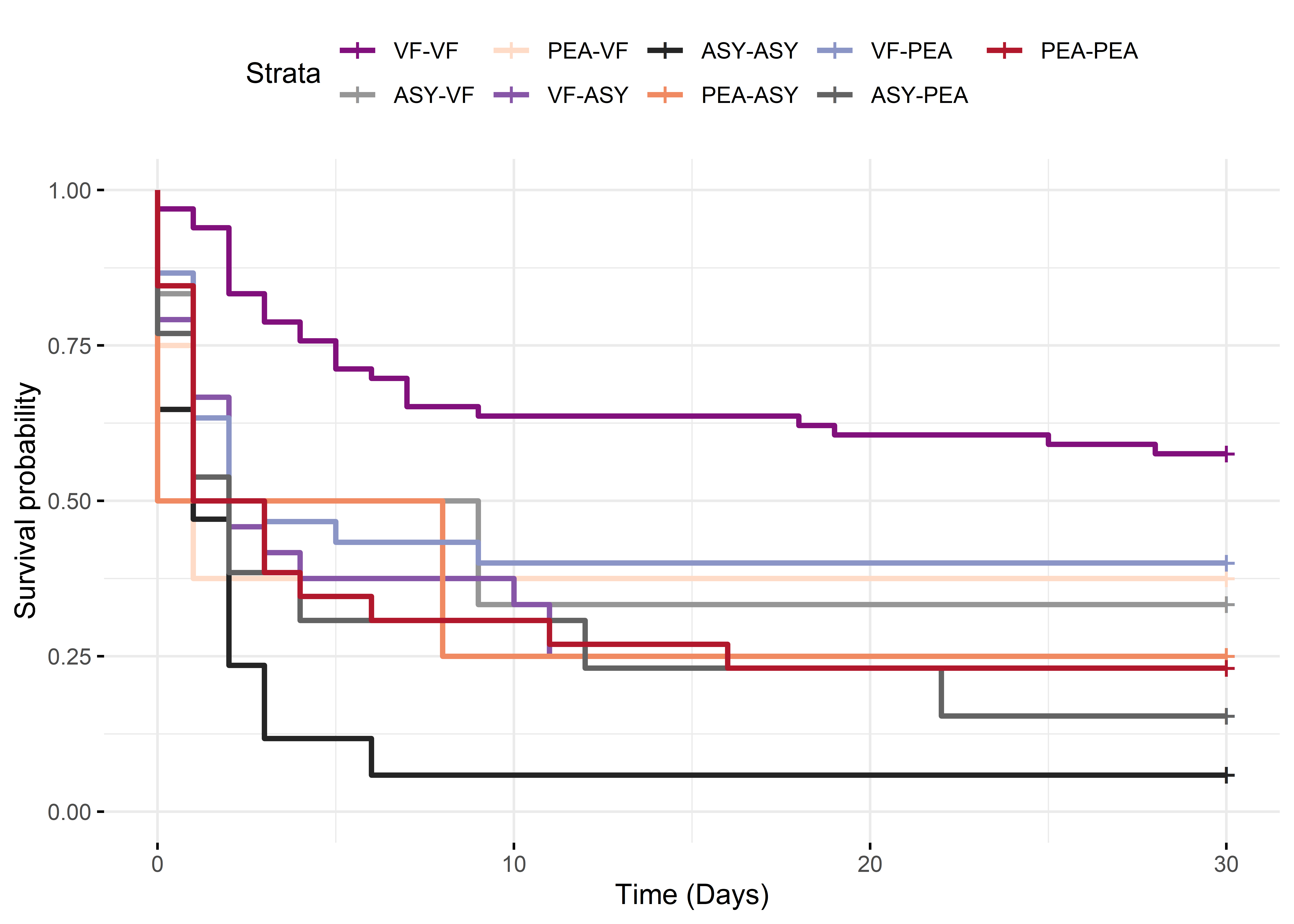
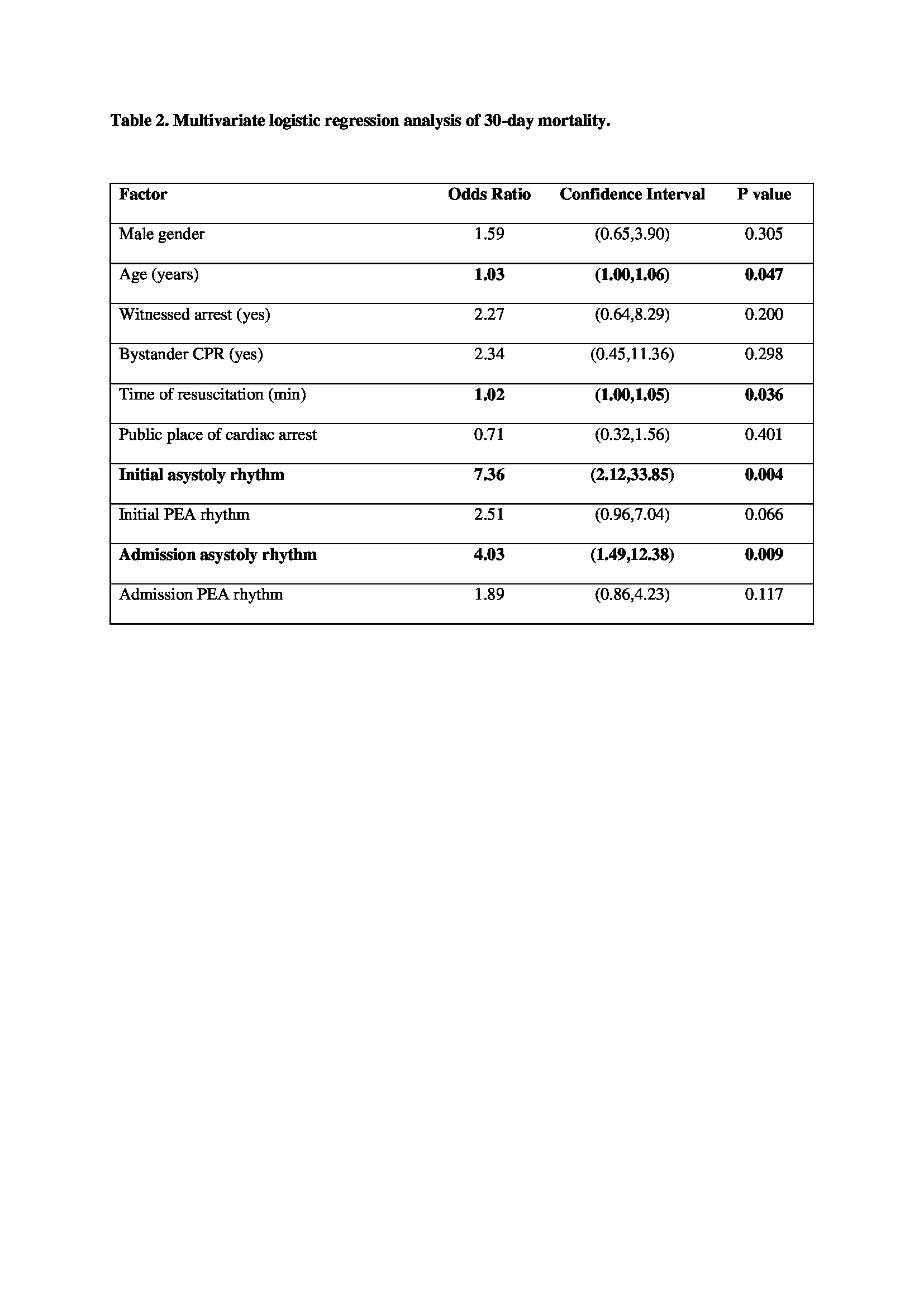
Results: From January 2012 to December 2023, a total of 1,219 OHCA patients were admitted to the hospital, of whom 210 received ECPR. Of these, 196 patients were included in the final analysis. The mean age of the ECPR recipients was 52.9 (±13) years, with 80.6% being male, and the median time to ECPR initiation was 61 (IQR 54-72) minutes. Patients presenting with ventricular fibrillation as both the initial rhythm and the rhythm at hospital arrival exhibited the highest 30-day survival rate (35/67, 52%), whereas those presenting with asystole as both the initial rhythm and the rhythm at hospital arrival had the lowest survival rate (1/17, 6%, log-rank p<0.00001). After adjusting for age, sex, initial rhythm, time of resuscitation, place, bystander and witnessed status, asystole at hospital arrival was associated with higher 30-day mortality (OR 4.03, 95% CI 1.49-12.38, p=0.009) and a poor neurological outcome at discharge, defined as a Cerebral Performance Category 3-5 (OR 4.61, 95% CI 1.49-17.62, p=0.013).
Conclusions: The heart rhythm at hospital admission is associated with outcomes in ECPR recipients. Patients who present and remain in ventricular fibrillation have a reasonable chance of favorable neurological survival. Conversely, patients who present in or convert to asystole have poor outcomes. The rhythm at hospital admission appears to be a valuable criterion for deciding whether to initiate ECPR.
Methods: In this prospective, observational, single-center registry study, the impact of the rhythm at hospital admission (ventricular fibrillation, pulseless electrical activity, or asystole) on 30-day survival and neurological outcomes at discharge was evaluated among patients who received ECPR for out-of-hospital cardiac arrest (OHCA).
Results: From January 2012 to December 2023, a total of 1,219 OHCA patients were admitted to the hospital, of whom 210 received ECPR. Of these, 196 patients were included in the final analysis. The mean age of the ECPR recipients was 52.9 (±13) years, with 80.6% being male, and the median time to ECPR initiation was 61 (IQR 54-72) minutes. Patients presenting with ventricular fibrillation as both the initial rhythm and the rhythm at hospital arrival exhibited the highest 30-day survival rate (35/67, 52%), whereas those presenting with asystole as both the initial rhythm and the rhythm at hospital arrival had the lowest survival rate (1/17, 6%, log-rank p<0.00001). After adjusting for age, sex, initial rhythm, time of resuscitation, place, bystander and witnessed status, asystole at hospital arrival was associated with higher 30-day mortality (OR 4.03, 95% CI 1.49-12.38, p=0.009) and a poor neurological outcome at discharge, defined as a Cerebral Performance Category 3-5 (OR 4.61, 95% CI 1.49-17.62, p=0.013).
Conclusions: The heart rhythm at hospital admission is associated with outcomes in ECPR recipients. Patients who present and remain in ventricular fibrillation have a reasonable chance of favorable neurological survival. Conversely, patients who present in or convert to asystole have poor outcomes. The rhythm at hospital admission appears to be a valuable criterion for deciding whether to initiate ECPR.
More abstracts on this topic:
Catastrophic Bioprosthetic Aortic Valve Thrombosis: An Unappreciated Complication of Veno-Arterial Extracorporeal Membrane Oxygenation Support in Cardiogenic Shock
O'hara Patrick, Heid Christopher, Lahsaei Peiman, Farr Maryjane, Garg Sonia, Araj Faris, Truby Lauren, Goral Montana, Kim Han, Malensek Paris, Beaini Hadi, Patel Ravi, Jawaid Anas, Hussain Fizza
A Recalled Experience of Death Among Cardiac Arrest Survivors Is Associated with Improved Psychological OutcomesGoins Imani, Ingram Cambell, Wei Lijing, Gonzales Anelly, He Tun, Moore Sacha, Parnia Sam