Final ID: LBOr04
The Association between Bystander-Performed Chest Compression Strategy and Neurological Outcomes for Opioid-Associated and Undifferentiated Out-of-Hospital Cardiac Arrest
Abstract Body: Background: Previous studies support bystander provision of chest compression-only CPR (CC-CPR) for out-of-hospital cardiac arrest (OHCA). However, OHCA secondary to opioid toxicity may benefit from chest compression-plus-ventilation CPR (CCV-CPR). We examined the association between different bystander CPR strategies and clinical outcomes among opioid-associated (OA-OHCA) or undifferentiated OHCA’s.
Methods: We included adult OHCAs treated by emergency medical services (EMS) from the BC Cardiac Arrest Registry (Dec/2014-Mar/2020), excluding EMS-witnessed cases. We classified cases as “OA-OHCA” based on positive post-mortem toxicological testing, death certificates with opioid toxicity as cause-of-death, or opioid-specific hospital-based diagnoses. We fit a multivariable logistic regression model for complete cases to assess the association of bystander CPR strategy (CC-CPR [reference] vs. CCV-CPR and no CPR) on survival with favourable neurological outcome (CPC 1-2) at hospital discharge; we included an interaction term between OA-OHCA and bystander CPR strategy to show results among OA-OHCA and undifferentiated OHCA cases separately.
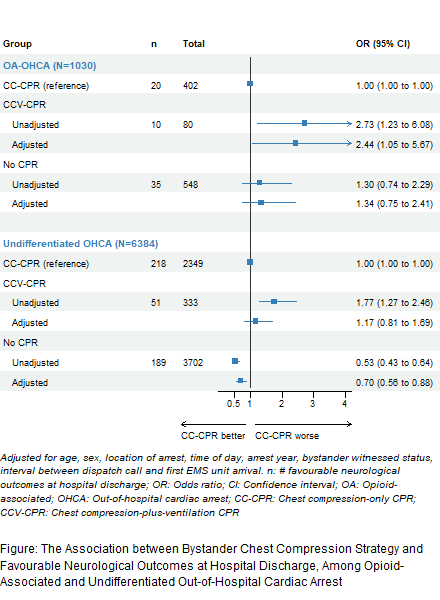
Results: We included 10,899 cases. CC-CPR, CCV-CPR, unknown CPR strategy, and no bystander CPR was performed in 2908 (27%), 437 (4.0%), 3123 (29%), and 4431 (41%) cases, respectively. Of OA-OHCAs (n=1350), the median age was 39 years (IQR 31-51), 327 (24%) were female, and 1055 (78%) were in private locations. Of undifferentiated OHCA (n=9549), the median age was 70 years (IQR 58-81), 2912 (31%) were female, and 7530 (79%) were in private locations. Our complete-case model (n=7414; Figure) showed that among OA-OHCA: with reference to CC-CPR, CCV-CPR was associated with improved outcomes (adjusted OR 2.44, 95% CI 1.05, 5.67), but an association with no CPR was not detected (adjusted OR 1.34, 95% CI 0.75, 2.41). Among undifferentiated OHCAs: with reference to CC-CPR, an association with CCV-CPR was not detected (adjusted OR 1.17, 95% CI 0.81, 1.69), but no CPR was associated with worse outcomes (adjusted OR 0.70, 95% CI 0.56, 0.88). The interaction term was not significant (p=0.09).
Conclusion: Our study suggests that bystander CCV-CPR, compared to CC-CPR, is associated with improved outcomes in OA-OHCA, but not for undifferentiated OHCA. Among OA-OHCA, outcomes of those receiving CC-CPR and no CPR appeared similar. These data suggest that ventilations may play a key role in bystander OA-OHCA resuscitation.
Methods: We included adult OHCAs treated by emergency medical services (EMS) from the BC Cardiac Arrest Registry (Dec/2014-Mar/2020), excluding EMS-witnessed cases. We classified cases as “OA-OHCA” based on positive post-mortem toxicological testing, death certificates with opioid toxicity as cause-of-death, or opioid-specific hospital-based diagnoses. We fit a multivariable logistic regression model for complete cases to assess the association of bystander CPR strategy (CC-CPR [reference] vs. CCV-CPR and no CPR) on survival with favourable neurological outcome (CPC 1-2) at hospital discharge; we included an interaction term between OA-OHCA and bystander CPR strategy to show results among OA-OHCA and undifferentiated OHCA cases separately.
Results: We included 10,899 cases. CC-CPR, CCV-CPR, unknown CPR strategy, and no bystander CPR was performed in 2908 (27%), 437 (4.0%), 3123 (29%), and 4431 (41%) cases, respectively. Of OA-OHCAs (n=1350), the median age was 39 years (IQR 31-51), 327 (24%) were female, and 1055 (78%) were in private locations. Of undifferentiated OHCA (n=9549), the median age was 70 years (IQR 58-81), 2912 (31%) were female, and 7530 (79%) were in private locations. Our complete-case model (n=7414; Figure) showed that among OA-OHCA: with reference to CC-CPR, CCV-CPR was associated with improved outcomes (adjusted OR 2.44, 95% CI 1.05, 5.67), but an association with no CPR was not detected (adjusted OR 1.34, 95% CI 0.75, 2.41). Among undifferentiated OHCAs: with reference to CC-CPR, an association with CCV-CPR was not detected (adjusted OR 1.17, 95% CI 0.81, 1.69), but no CPR was associated with worse outcomes (adjusted OR 0.70, 95% CI 0.56, 0.88). The interaction term was not significant (p=0.09).
Conclusion: Our study suggests that bystander CCV-CPR, compared to CC-CPR, is associated with improved outcomes in OA-OHCA, but not for undifferentiated OHCA. Among OA-OHCA, outcomes of those receiving CC-CPR and no CPR appeared similar. These data suggest that ventilations may play a key role in bystander OA-OHCA resuscitation.
More abstracts on this topic:
A Multicentre Study for Hands Only CPR (HOCPR) training assessment towards building a ‘Nation of Life Savers” in India
Ravikumar Thanjavur, Sarma Kvs, Ravikumar Thanjavur, Sarkar Manuj, Debnath Dhrubajyoti, Behera Priyamadhaba, Ghate Jayshri, Trikha Divay, Samantaray A, Madhavi K
A Porcine Model of Cardiac Arrest Without Pre-Arrest Fluid Loading, Sternal Molding, or EpinephrineParadis Aidan, Paradis Norman, Gaddy David, Moodie Karen, Mader Timothy, Dufresne Alexandre, Couturier Christine, Dufresne Simon, Davis Daniel, Sims Christopher