Final ID: Sa1101
Association Between Changes in Hypoxic-Ischemic Brain Injury and Neurological Outcomes in Cardiac Arrest Survivors.
Abstract Body: Aim: Quantitative analysis of hypoxic-ischemic brain injury (HIBI) using apparent diffusion coefficient (ADC) values from brain magnetic resonance imaging (MRI) is used to predict poor neurological outcomes in out-of-hospital cardiac arrest (OHCA) survivors. Our study aimed to determine the association between changes in HIBI and neurological outcomes in OHCA survivors using two types of MRI.
Methods: This observational study used data collected prospectively from a tertiary academic hospital. The study included adult comatose OHCA survivors who underwent targeted temperature management (TTM) and brain MRI within 6 hours (first) and 72–96 hours (second) using the same MR scanner. We analyzed the neurological outcomes based on brain volumes below a specific ADC value using 10-step intervals within the range of 200–1200 × 10-6mm2/s for the first and second MRIs. ADC-R(x) represents the proportion of total brain volume occupied by voxels, with ADC values ranging from 200 × 10-6mm2/s to each threshold. Additionally, ADC(x) represents the proportion of total brain volume occupied by voxels that are “threshold - 10” at each threshold.
Poor neurological outcomes were categorized as cerebral performance levels 3–5, observed 6 months after OHCA.
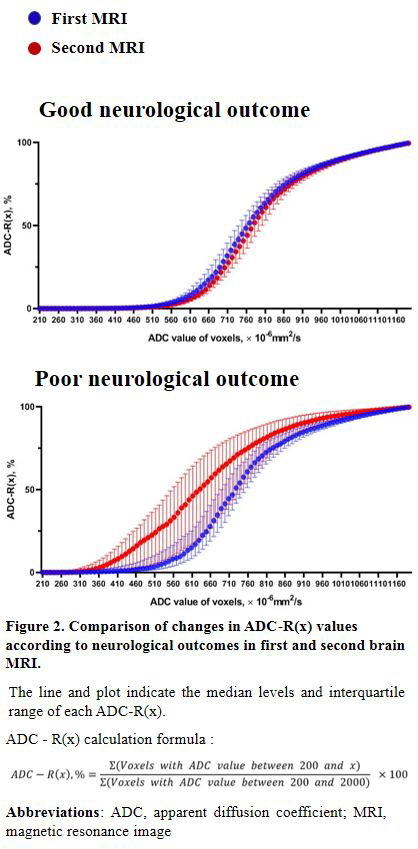
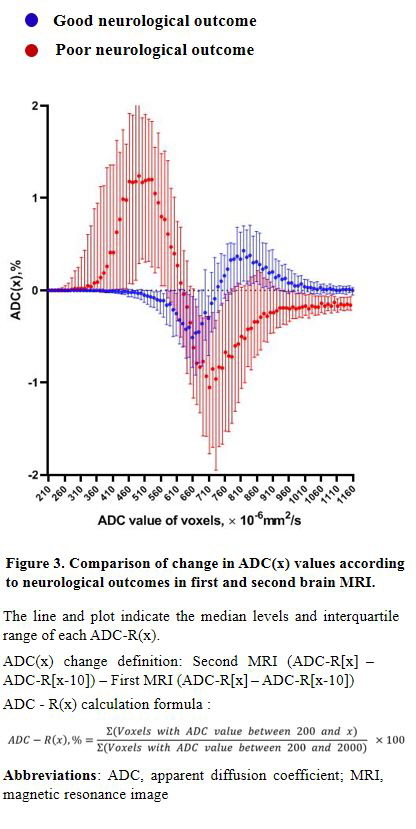
Results: Overall, 122 patients (25% female) were included in the analysis, of whom 61 (50%) showed poor neurological outcomes. Higher ADC-R(x) were observed in the poor neurological outcome group on both the first and second MRI scans at all ADC intervals (all P < 0.05) (Figure 1). In the Good Neurological Outcome group, the ADC-R values ranged between 370 and 940, with the second MRI value being smaller than that of the first (right shift, P < 0.05). In contrast, the Poor Neurological Outcome group showed ADC-R values ranging between 340 and 1190, with the second MRI value being higher than that of the first (left shift, P < 0.05) (Figure 2). The difference in ADC(x) between the second and first MRI based on neurological outcome showed a positive change in ADC below 620 for a poor neurological outcome and a positive change in ADC above 740 for a good neurological outcome (Figure 3).
Conclusions: In this cohort study, we observed that the initial HIBI that occurred during OHCA worsened or returned to normal depending on the neurological outcome after TTM. Prospective multicenter studies are required to generalize our findings.
Methods: This observational study used data collected prospectively from a tertiary academic hospital. The study included adult comatose OHCA survivors who underwent targeted temperature management (TTM) and brain MRI within 6 hours (first) and 72–96 hours (second) using the same MR scanner. We analyzed the neurological outcomes based on brain volumes below a specific ADC value using 10-step intervals within the range of 200–1200 × 10-6mm2/s for the first and second MRIs. ADC-R(x) represents the proportion of total brain volume occupied by voxels, with ADC values ranging from 200 × 10-6mm2/s to each threshold. Additionally, ADC(x) represents the proportion of total brain volume occupied by voxels that are “threshold - 10” at each threshold.
Poor neurological outcomes were categorized as cerebral performance levels 3–5, observed 6 months after OHCA.
Results: Overall, 122 patients (25% female) were included in the analysis, of whom 61 (50%) showed poor neurological outcomes. Higher ADC-R(x) were observed in the poor neurological outcome group on both the first and second MRI scans at all ADC intervals (all P < 0.05) (Figure 1). In the Good Neurological Outcome group, the ADC-R values ranged between 370 and 940, with the second MRI value being smaller than that of the first (right shift, P < 0.05). In contrast, the Poor Neurological Outcome group showed ADC-R values ranging between 340 and 1190, with the second MRI value being higher than that of the first (left shift, P < 0.05) (Figure 2). The difference in ADC(x) between the second and first MRI based on neurological outcome showed a positive change in ADC below 620 for a poor neurological outcome and a positive change in ADC above 740 for a good neurological outcome (Figure 3).
Conclusions: In this cohort study, we observed that the initial HIBI that occurred during OHCA worsened or returned to normal depending on the neurological outcome after TTM. Prospective multicenter studies are required to generalize our findings.
More abstracts on this topic:
A Patient and Family Advisory Council After Cardiac Arrest: A Patient-Centered Model of Community Engagement
Riker Richard, Chessa Frank, Sawyer Douglas, Seder David B., Weatherbee Mary, Daley Alison, Searight Meghan, Lord Christine, Lessard Amanda, Feutz Catherine, May Teresa, Gagnon David
A Multicentre Study for Hands Only CPR (HOCPR) training assessment towards building a ‘Nation of Life Savers” in IndiaRavikumar Thanjavur, Sarma Kvs, Ravikumar Thanjavur, Sarkar Manuj, Debnath Dhrubajyoti, Behera Priyamadhaba, Ghate Jayshri, Trikha Divay, Samantaray A, Madhavi K