Final ID: Sa806
Prognostic Predictions after Pediatric Cardiac Arrest: A Single Center Prospective Study
Abstract Body: BACKGROUND:
Almost half of children who have a cardiac arrest die after withdrawal of life sustaining therapy (WLST), which is influenced by provider outcome predictions. Clinical factors used by providers to predict outcomes after pediatric cardiac arrest and the prognostic accuracy of providers are not known.
AIMS:
We describe clinical factors providers report using to predict outcomes in the first week post-arrest and determine the concordance of prognostic predictions with patient outcome at hospital discharge.
HYPOTHESIS:
We hypothesized that the use of post-arrest factors would increase within the first week and that the concordance of prognostic predictions with patient outcome would increase over time from return of circulation (ROC).
METHODS:
This is a single-center prospective cohort study from 7/2023 to 4/2024. We included children with an index pediatric in-hospital (IHCA) or out-of-hospital (OHCA) cardiac arrest with ROC who received post-arrest care in the PICU. Multidisciplinary team members completed real-time surveys on post-arrest days 1, 2, 3, and 7. Surveys assessed provider demographics, top 3 factors used to form their prediction, and prediction of patient discharge outcome (Pediatric Cerebral Performance Category [PCPC] score). Actual outcome was PCPC at hospital discharge or 30 days, whichever was later, and was compared to provider prediction. Prognostic concordance is defined in Table 3. Mixed-effect models explored changes in factors used for prediction and concordance between prognostic predictions and patient outcomes over survey time points.
RESULTS:
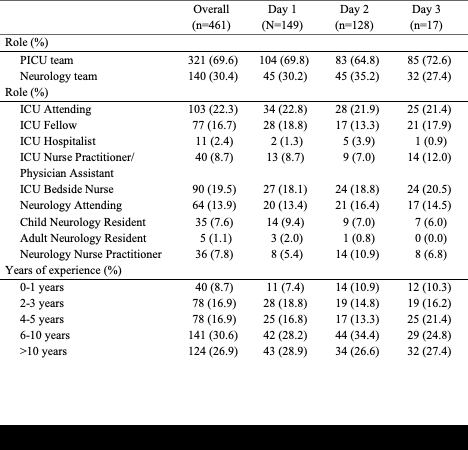
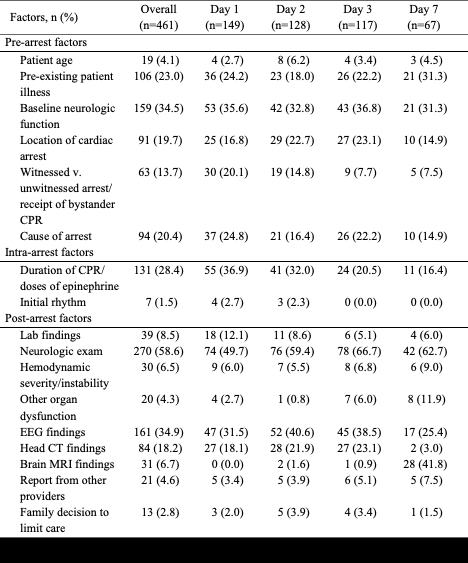
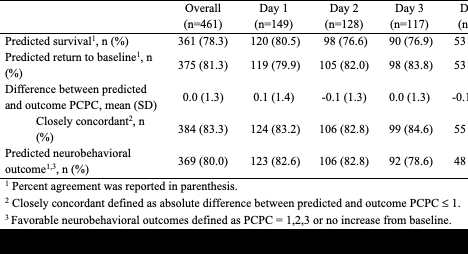
Fifty cardiac patients (median age: 4 years [IQR: 1, 10], 60% OHCA, and 52% pre-arrest PCPC = 1) were analyzed; survival at discharge/30 days was 76%. There were 461 surveys completed by 217 providers (Table 1). Over all survey time points, the top 3 factors reported to predict outcomes were pre-arrest neurologic function, post-arrest neurologic exam and EEG (Table 2). Use of neurologic exam, other organ dysfunction, and MRI findings increased over the first 3 days, OR 1.6 (95% CI 1.2-2.2). More than 75% of provider predictions were concordant with the actual outcome, by all definitions, with no significant change over the first week (Table 3).
CONCLUSIONS:
During the first week post-arrest, providers report increasing incorporation of the post arrest factors to prognosticate outcomes. Concordance of outcome prediction was more than 75% and did not change over the first week.
Almost half of children who have a cardiac arrest die after withdrawal of life sustaining therapy (WLST), which is influenced by provider outcome predictions. Clinical factors used by providers to predict outcomes after pediatric cardiac arrest and the prognostic accuracy of providers are not known.
AIMS:
We describe clinical factors providers report using to predict outcomes in the first week post-arrest and determine the concordance of prognostic predictions with patient outcome at hospital discharge.
HYPOTHESIS:
We hypothesized that the use of post-arrest factors would increase within the first week and that the concordance of prognostic predictions with patient outcome would increase over time from return of circulation (ROC).
METHODS:
This is a single-center prospective cohort study from 7/2023 to 4/2024. We included children with an index pediatric in-hospital (IHCA) or out-of-hospital (OHCA) cardiac arrest with ROC who received post-arrest care in the PICU. Multidisciplinary team members completed real-time surveys on post-arrest days 1, 2, 3, and 7. Surveys assessed provider demographics, top 3 factors used to form their prediction, and prediction of patient discharge outcome (Pediatric Cerebral Performance Category [PCPC] score). Actual outcome was PCPC at hospital discharge or 30 days, whichever was later, and was compared to provider prediction. Prognostic concordance is defined in Table 3. Mixed-effect models explored changes in factors used for prediction and concordance between prognostic predictions and patient outcomes over survey time points.
RESULTS:
Fifty cardiac patients (median age: 4 years [IQR: 1, 10], 60% OHCA, and 52% pre-arrest PCPC = 1) were analyzed; survival at discharge/30 days was 76%. There were 461 surveys completed by 217 providers (Table 1). Over all survey time points, the top 3 factors reported to predict outcomes were pre-arrest neurologic function, post-arrest neurologic exam and EEG (Table 2). Use of neurologic exam, other organ dysfunction, and MRI findings increased over the first 3 days, OR 1.6 (95% CI 1.2-2.2). More than 75% of provider predictions were concordant with the actual outcome, by all definitions, with no significant change over the first week (Table 3).
CONCLUSIONS:
During the first week post-arrest, providers report increasing incorporation of the post arrest factors to prognosticate outcomes. Concordance of outcome prediction was more than 75% and did not change over the first week.
More abstracts on this topic:
Brain Oxygen and ICP Optimization in Severe post Cardiac Arrest (BOOSCA)
Seder David B., Lord Christine, Searight Meghan, Higgins Bethany, Joyce Maura, Gallant Betsey, Huff Talena, May Teresa, Brennan Julia, Weatherbee Mary, Wishengrad Jeanne, Riker Richard, Gagnon David, Michalakes Peter, Ryzhov Sergey, Dekay Joanne
A Polypill Strategy for Heart Failure with Reduced Ejection Fraction: The POLY-HF TrialPandey Ambarish, Wang Thomas, Keshvani Neil, Rizvi Syed Kazim, Jain Anand, Coellar Juan David, Drazner Mark, Gupta Deepak, Chandra Alvin, Zaha Vlad