Final ID: Sa802
Why Physicians Use Sodium Bicarbonate During Cardiac Arrest: A Mixed Methods Survey of Adult and Pediatric Clinicians
Abstract Body: Background: Despite national recommendations against the routine use of sodium bicarbonate (SB) during cardiac arrest, SB is used in about 50% of both pediatric and adult IHCA, making it the second most used drug, after epinephrine.
Aims: To explore clinician practices and beliefs surrounding intra-arrest SB administration.
Hypothesis: We hypothesized that SB use would vary by specialty, and that indications for intra-arrest SB not endorsed by AHA guidelines would be common.
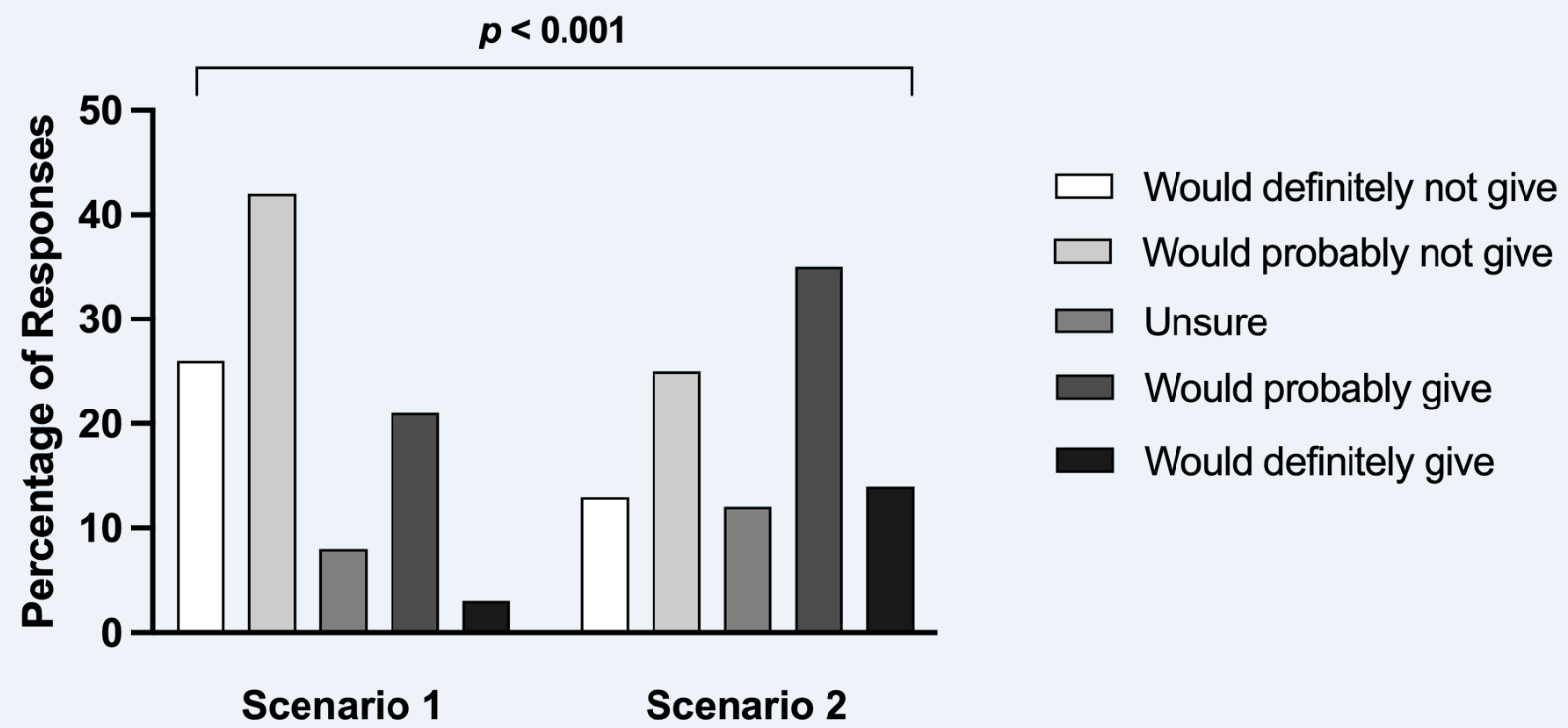
Methods: We performed a mixed methods electronic survey amongst adult and pediatric intensive care unit (ICU), emergency medicine (EM) and anesthesia attendings at two local institutions in Boston, MA from October 3rd to December 15th, 2023. Likert scale responses for likelihood of giving SB in 2 cardiac arrest scenarios were compared using a Chi-squared test. These responses were dichotomized to reflect those who would “probably” or “definitely” give SB versus those who would not, and respondent characteristics were compared. For the open-ended items, we performed qualitative thematic analysis.
Results: Of 356 physicians invited, 224 (63%) responded. The likelihood of giving SB in Scenario 1 (10-minute asystolic arrest) and Scenario 2 (20-minute asystolic arrest) differed (Figure 1), with 54/224 (24%) respondents indicating they would give SB in Scenario 1 and 110 (49%) for Scenario 2. Additionally, likelihood of giving SB in Scenario 1 varied based on practice location (p = 0.025) with the lowest rates in pediatric and adult EM (8% and 10%, respectively) and the highest amongst those in adult ICUs (38%). These differences persisted for Scenario 2 (p = 0.001). SB use in Scenario 1 also decreased with increasing years of experience (p = 0.032). The most reported indications for SB were: hyperkalemia (78%); metabolic acidosis (76%) with a median reported threshold pH of 7.1 (IQR: 7, 7.2); tricyclic anti-depressant overdose (71%); and arrest duration (64%) with a median reported threshold of 15 minutes (IQR: 10, 20). In the qualitative analysis, additional themes emerged for reasons respondents give SB, including specific diagnoses, arrest rhythms, team dynamics and beliefs about the physiological effects of SB.
Conclusions: Physicians reported significant practice variations surrounding cardiac arrest management with SB, including several indications for SB which are not supported by national cardiac arrest guidelines.
Aims: To explore clinician practices and beliefs surrounding intra-arrest SB administration.
Hypothesis: We hypothesized that SB use would vary by specialty, and that indications for intra-arrest SB not endorsed by AHA guidelines would be common.
Methods: We performed a mixed methods electronic survey amongst adult and pediatric intensive care unit (ICU), emergency medicine (EM) and anesthesia attendings at two local institutions in Boston, MA from October 3rd to December 15th, 2023. Likert scale responses for likelihood of giving SB in 2 cardiac arrest scenarios were compared using a Chi-squared test. These responses were dichotomized to reflect those who would “probably” or “definitely” give SB versus those who would not, and respondent characteristics were compared. For the open-ended items, we performed qualitative thematic analysis.
Results: Of 356 physicians invited, 224 (63%) responded. The likelihood of giving SB in Scenario 1 (10-minute asystolic arrest) and Scenario 2 (20-minute asystolic arrest) differed (Figure 1), with 54/224 (24%) respondents indicating they would give SB in Scenario 1 and 110 (49%) for Scenario 2. Additionally, likelihood of giving SB in Scenario 1 varied based on practice location (p = 0.025) with the lowest rates in pediatric and adult EM (8% and 10%, respectively) and the highest amongst those in adult ICUs (38%). These differences persisted for Scenario 2 (p = 0.001). SB use in Scenario 1 also decreased with increasing years of experience (p = 0.032). The most reported indications for SB were: hyperkalemia (78%); metabolic acidosis (76%) with a median reported threshold pH of 7.1 (IQR: 7, 7.2); tricyclic anti-depressant overdose (71%); and arrest duration (64%) with a median reported threshold of 15 minutes (IQR: 10, 20). In the qualitative analysis, additional themes emerged for reasons respondents give SB, including specific diagnoses, arrest rhythms, team dynamics and beliefs about the physiological effects of SB.
Conclusions: Physicians reported significant practice variations surrounding cardiac arrest management with SB, including several indications for SB which are not supported by national cardiac arrest guidelines.
More abstracts on this topic:
Assessment of Guideline-Recommended Treatment Times for ST-Elevation Myocardial Infarction Across Critical Access Hospital Networks
Brock Aiden, Campos-staffico Alessandra
Cardiac RBFOX1 Deficiency Enhances Glucose and Ketone Metabolism and Provides Tolerance Against Ischemia Reperfusion InjuryTejay Saymon, Michelakis Evangelos, Hannington Patrick, Ussher John, Sutendra Gopinath, Chan Jordan, Wagg Cory, Nanoa Joseph, Lorenzana Maria Areli, Liu Yongsheng, Zhao Yuan Yuan, Hambrook Jacob, Bowhay Christina