Final ID: LBP48
Impact of Anti-Vascular Endothelial Growth Factor Agents in Patients with Chronic Subdural Hematoma
Abstract Body: Objective: To assess the effects of anti-VEGF agents on clinical outcomes in chronic subdural hematoma (cSDH) patients.
Methods: We conducted a retrospective cohort study using the TriNetX database, comparing cSDH patients treated with anti-VEGF agents to untreated controls. Propensity score matching adjusted for demographics, comorbidities, neoplasms, and medication use, excluding acute subdural hematoma and CNS malignancies. Outcomes at 6-month and 1-year follow-ups included incidence of headache, rebleeding, surgical intervention (open craniotomy, burr holes, endovascular embolization), mortality, hypertension, major bleeding, acute kidney failure, and stroke.
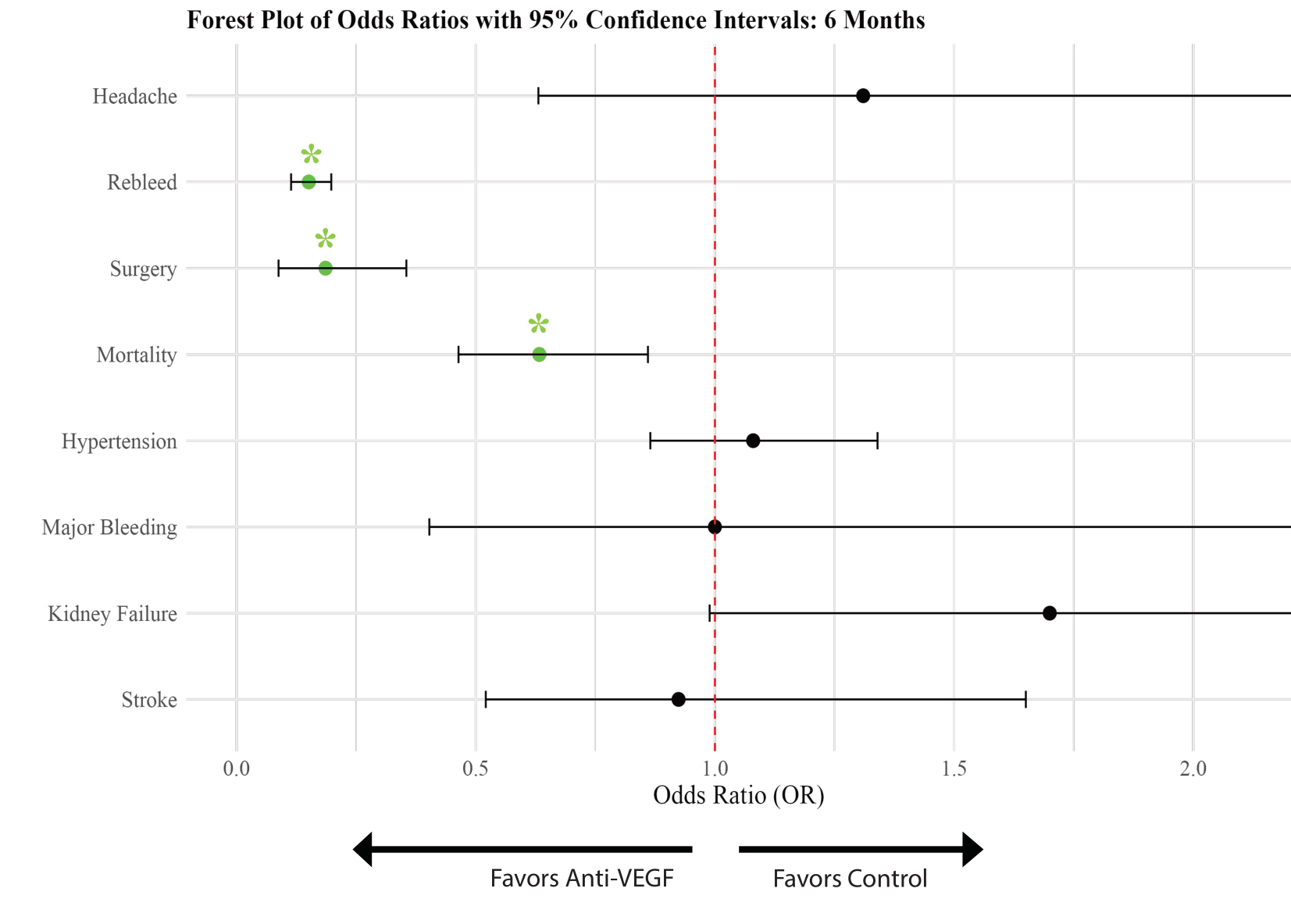
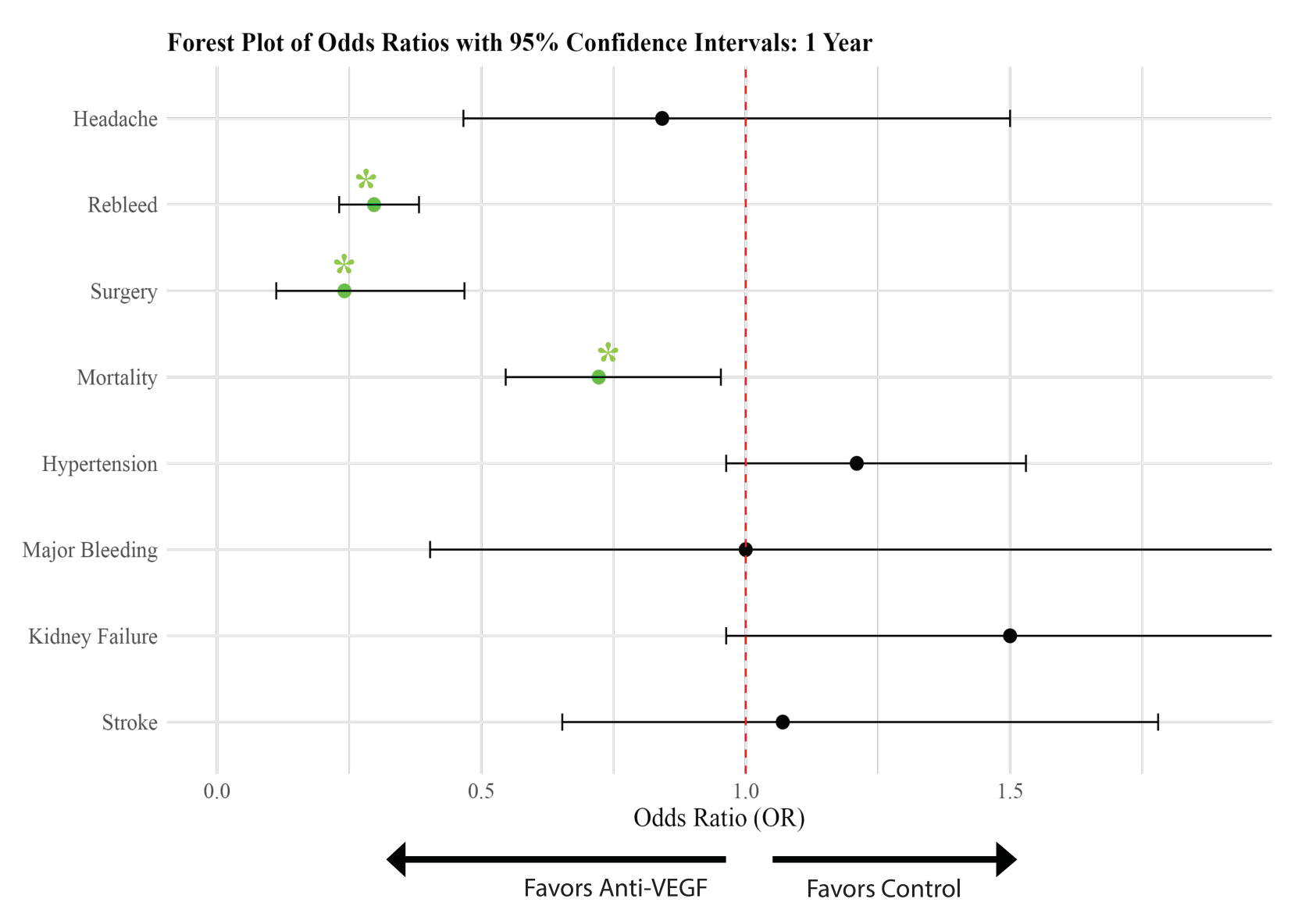
Results: At 6 months (n = 644 per group), anti-VEGF treatment was associated with reduced rebleeding (OR = 0.151; 95% CI: 0.114–0.198; p < 0.001), fewer surgical interventions (OR = 0.186; 95% CI: 0.088–0.355; p < 0.001), and lower mortality (OR = 0.633; 95% CI: 0.464–0.860; p = 0.003). Headache incidence was similar between groups (OR = 1.31; 95% CI: 0.631–2.800; p = 0.999). At 1 year (n = 620 per group), anti-VEGF therapy continued to show associations with reduced rebleeding (OR = 0.297; 95% CI: 0.231–0.382; p < 0.001), lower need for surgery (OR = 0.241; 95% CI: 0.112–0.468; p < 0.001), and reduced mortality (OR = 0.722; 95% CI: 0.546–0.953; p = 0.023). Headache incidence remained non-significant (OR = 0.842; 95% CI: 0.466–1.500; p = 0.561). No significant differences were observed in hypertension (6 months: OR = 1.07; 95% CI: 0.865–1.340; p = 0.501; 1 year: OR = 1.210; 95% CI: 0.963–1.530; p = 0.101), major bleeding (6 months and 1 year: OR = 1.00; 95% CI: 0.403–2.480; p = 0.999), acute kidney failure (6 months: OR = 1.700; 95% CI: 0.989–3.000; p = 0.055; 1 year: OR = 1.500; 95% CI: 0.963–2.360; p = 0.073), or stroke (6 months: OR = 0.924; 95% CI: 0.521–1.650; p = 0.788; 1 year: OR = 1.070; 95% CI: 0.653–1.780; p = 0.787).
Conclusion: Anti-VEGF therapy in cSDH shows potential in reducing rebleeding, surgical intervention needs, and mortality. The unchanged incidence of headaches might reflect the high baseline prevalence. Additionally, the risk of complications commonly associated with anti-VEGF was not significant. While these findings suggest clinical benefits, further research is needed to validate these outcomes and fully assess the role of anti-VEGF in cSDH management.
Methods: We conducted a retrospective cohort study using the TriNetX database, comparing cSDH patients treated with anti-VEGF agents to untreated controls. Propensity score matching adjusted for demographics, comorbidities, neoplasms, and medication use, excluding acute subdural hematoma and CNS malignancies. Outcomes at 6-month and 1-year follow-ups included incidence of headache, rebleeding, surgical intervention (open craniotomy, burr holes, endovascular embolization), mortality, hypertension, major bleeding, acute kidney failure, and stroke.
Results: At 6 months (n = 644 per group), anti-VEGF treatment was associated with reduced rebleeding (OR = 0.151; 95% CI: 0.114–0.198; p < 0.001), fewer surgical interventions (OR = 0.186; 95% CI: 0.088–0.355; p < 0.001), and lower mortality (OR = 0.633; 95% CI: 0.464–0.860; p = 0.003). Headache incidence was similar between groups (OR = 1.31; 95% CI: 0.631–2.800; p = 0.999). At 1 year (n = 620 per group), anti-VEGF therapy continued to show associations with reduced rebleeding (OR = 0.297; 95% CI: 0.231–0.382; p < 0.001), lower need for surgery (OR = 0.241; 95% CI: 0.112–0.468; p < 0.001), and reduced mortality (OR = 0.722; 95% CI: 0.546–0.953; p = 0.023). Headache incidence remained non-significant (OR = 0.842; 95% CI: 0.466–1.500; p = 0.561). No significant differences were observed in hypertension (6 months: OR = 1.07; 95% CI: 0.865–1.340; p = 0.501; 1 year: OR = 1.210; 95% CI: 0.963–1.530; p = 0.101), major bleeding (6 months and 1 year: OR = 1.00; 95% CI: 0.403–2.480; p = 0.999), acute kidney failure (6 months: OR = 1.700; 95% CI: 0.989–3.000; p = 0.055; 1 year: OR = 1.500; 95% CI: 0.963–2.360; p = 0.073), or stroke (6 months: OR = 0.924; 95% CI: 0.521–1.650; p = 0.788; 1 year: OR = 1.070; 95% CI: 0.653–1.780; p = 0.787).
Conclusion: Anti-VEGF therapy in cSDH shows potential in reducing rebleeding, surgical intervention needs, and mortality. The unchanged incidence of headaches might reflect the high baseline prevalence. Additionally, the risk of complications commonly associated with anti-VEGF was not significant. While these findings suggest clinical benefits, further research is needed to validate these outcomes and fully assess the role of anti-VEGF in cSDH management.
More abstracts on this topic:
A 10-year longitudinal cohort study of lipid variability, cognitive decline, and dementia in 9846 community-dwelling older adults
Zhou Zhen, Moran Chris, Murray Anne, Zoungas Sophia, Nelson Mark, Talic Stella, Wolfe Rory, Ryan Joanne
ADAR1 inhibiting ZBP1-driven neuronal necroptosis to improve secondary injury after intracerebral hemorrhageWang Shuoyang, Zhao Shoucai, Wu Xiaodong, Chu Zhaohu, Xu Yang
Readers' Comments
We encourage you to enter the discussion by posting your comments and questions below.
Presenters will be notified of your post so that they can respond as appropriate.
This discussion platform is provided to foster engagement, and simulate conversation and knowledge sharing.
You have to be authorized to post a comment. Please, Login or Signup.
Rate this abstract
(Maximum characters: 500)