Final ID: WP24
Symptomatic hemorrhage after thrombolysis: results from the Alteplase compared to Tenecteplase in patients with acute ischemic stroke trial
Abstract Body: Introduction: Because of the risk of infarcted tissue leading to symptomatic intracerebral hemorrhage (sICH) after intravenous thrombolysis for acute ischemic stroke, patients are monitored for at least 24 hours in a critical care setting. We aim to assess incidence and risk factors of sICH following thrombolysis for acute ischemic stroke. We hypothesize that the incidence of sICH is higher in patients with older age, longer symptom onset-to-needle (OTN), greater stroke severity, and lower baseline ASPECTS score.
Methods: Adults ≥18 years with acute ischemic stroke were randomized into the AcT trial to receive either intravenous TNK or tPA between December 2019 to January 2022 in 22 stroke centres in Canada. Patient demographics, stroke details, hemorrhagic complications (ICH, parenchymal hematoma, hemorrhagic infarct), and duration of hospital stay were collected. ANOVA and Chi-square tests compared demographic and clinical details across three groups: sICH, asymptomatic ICH (aICH), and no ICH (nICH). We developed logistic regression models to predict sICH and any ICH accounting for age, sex, pre-treatment NIHSS, OTN, baseline ASPECTS, and thrombolytic agent.
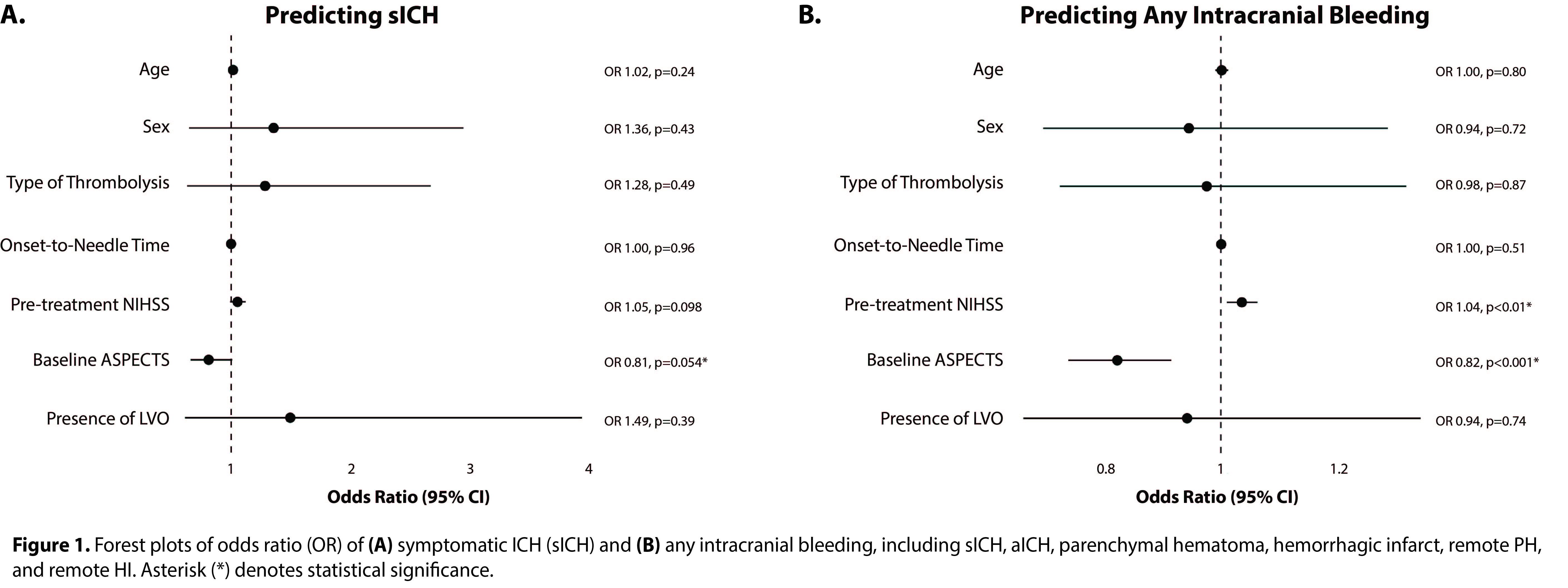
Preliminary Results: A total of 1556 participants were identified (sICH=51, aICH=261, nICH=1244). Mean age (72.02±14.2 years; p=0.11) and sex (48% female, p=0.13) were comparable between the groups. Mean pre-treatment NIHSS was highest in the sICH group (sICH 14.41±8.5, aICH 13.48±7.0, nICH 1055±6.6; p<0.001). Mean OTN was comparable across groups (sICH 141.90±62.6 min, aICH 142.65±65.1 min, nICH 144.46±69.5 min; p=0.90). Median ASPECTS was lower in the sICH group (sICH 8.00±1.7, aICH 9.00±1.6, nICH 9.00±1.4; p<0.001). There were higher odds of sICH with lower ASPECTS score (OR 0.81, 95% CI [0.66, 1], p=0.054). The risk of any intracranial hemorrhage was lower with higher ASPECTS score (OR 0.82, 95% CI [0.74, 0.91], p<0.001) and higher with worse NIHSS (OR 1.04, 95% CI [1.01, 1.06], p<0.01). Age, sex, OTN, and type of thrombolysis had no association with intracranial hemorrhage (Figure 1).
Conclusions: The risk of intracranial bleeding is greater when the infarct is more established and in patients with higher pre-treatment neurological deficit. Future analyses will seek to identify predictors of time to symptomatic bleeding, and to understand whether 24-hour ICU monitoring is needed for every recipient of thrombolysis.
Methods: Adults ≥18 years with acute ischemic stroke were randomized into the AcT trial to receive either intravenous TNK or tPA between December 2019 to January 2022 in 22 stroke centres in Canada. Patient demographics, stroke details, hemorrhagic complications (ICH, parenchymal hematoma, hemorrhagic infarct), and duration of hospital stay were collected. ANOVA and Chi-square tests compared demographic and clinical details across three groups: sICH, asymptomatic ICH (aICH), and no ICH (nICH). We developed logistic regression models to predict sICH and any ICH accounting for age, sex, pre-treatment NIHSS, OTN, baseline ASPECTS, and thrombolytic agent.
Preliminary Results: A total of 1556 participants were identified (sICH=51, aICH=261, nICH=1244). Mean age (72.02±14.2 years; p=0.11) and sex (48% female, p=0.13) were comparable between the groups. Mean pre-treatment NIHSS was highest in the sICH group (sICH 14.41±8.5, aICH 13.48±7.0, nICH 1055±6.6; p<0.001). Mean OTN was comparable across groups (sICH 141.90±62.6 min, aICH 142.65±65.1 min, nICH 144.46±69.5 min; p=0.90). Median ASPECTS was lower in the sICH group (sICH 8.00±1.7, aICH 9.00±1.6, nICH 9.00±1.4; p<0.001). There were higher odds of sICH with lower ASPECTS score (OR 0.81, 95% CI [0.66, 1], p=0.054). The risk of any intracranial hemorrhage was lower with higher ASPECTS score (OR 0.82, 95% CI [0.74, 0.91], p<0.001) and higher with worse NIHSS (OR 1.04, 95% CI [1.01, 1.06], p<0.01). Age, sex, OTN, and type of thrombolysis had no association with intracranial hemorrhage (Figure 1).
Conclusions: The risk of intracranial bleeding is greater when the infarct is more established and in patients with higher pre-treatment neurological deficit. Future analyses will seek to identify predictors of time to symptomatic bleeding, and to understand whether 24-hour ICU monitoring is needed for every recipient of thrombolysis.
More abstracts on this topic:
A Multicenter, Prospective, Randomized Controlled Trial of Endovascular Treatment with or without Intravenous ThromBolysis in Acute Ischemic Stroke of Basilar Artery Occlusion (BEST-BAO): Study Protocol
Xiang Yang, Siddiqui Adnan, Yang Shu, Mocco J, Yu Nengwei, Schonewille Wouter, Guo Fuqiang
A Novel Imaging Biomarker to Make Precise Outcome Predictions for Patients with Acute Ischemic StrokeMallavarapu Monica, Kim Hyun Woo, Iyyangar Ananya, Salazar-marioni Sergio, Yoo Albert, Giancardo Luca, Sheth Sunil, Jeevarajan Jerome
Readers' Comments
We encourage you to enter the discussion by posting your comments and questions below.
Presenters will be notified of your post so that they can respond as appropriate.
This discussion platform is provided to foster engagement, and simulate conversation and knowledge sharing.
You have to be authorized to post a comment. Please, Login or Signup.
Rate this abstract
(Maximum characters: 500)