Final ID: WMP35
Diagnostic and Therapeutic Challenges with Spinal Cord Infarction: A Real-World Experience from a Comprehensive Stroke Center
Abstract Body: Introduction: Spinal cord infarction (SCI) is a rare condition that accounts for only 1% to 2% of all ischemic strokes and 5% to 8% of acute myelopathies [1]. We aim to figure out the diagnostic and therapeutic challenges clinicians face with spinal cord infarction given scarcity of published data, overlapping clinical and neuroimaging findings with alternate etiologies for acute myelopathy, and utility of spinal diffusion weighted imaging (DWI) sequences in differentiating between different causes of acute myelopathy.
Methods and Material: Retrospective review of electronic medical records was done. Patients with discharge diagnosis of spinal stroke with DWI imaging evidence of infarction, challenging cases with positive DWI imaging but different pattern of clinical presentation and exam findings were included in the study. Cases without spinal DWI imaging were excluded.
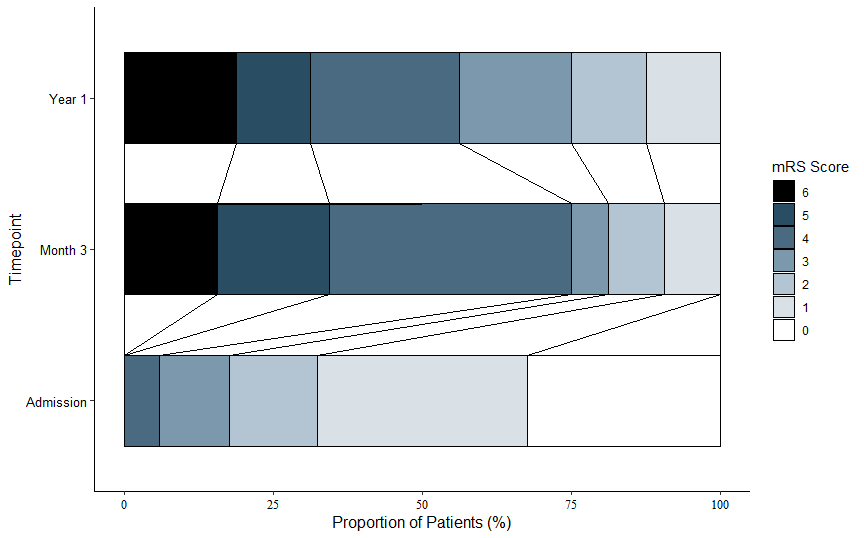
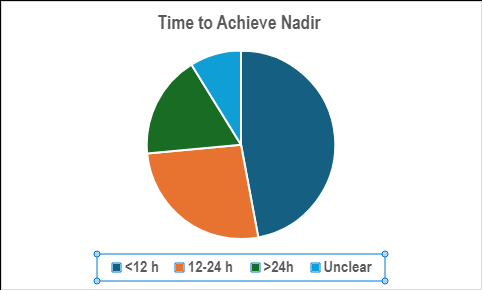
Results: Among the 34 DWI-positive patients included in the study with suspected SCI, the average age at presentation was 60 years, and 22 patients (64.7%) had vascular risk factors. A rapid onset of severe deficits, reaching their peak within 12 hours, was observed in 14 patients (41.1%), while 20 patients (58.8%) experienced a gradual decline. Sensory involvement was noted in 26 patients (76.4%), with 13 of these patients (50%) selectively retaining vibration and proprioception. Out of the 34 suspected SCI cases, 15 patients (44.1%) initially received alternative diagnoses, such as TM, NMOSD, Metastatic disease, Post-traumatic cord injury, or Post-laminectomy syndrome. However, after repeated imaging and continuous outpatient follow-up, 7 patients (46.6%) were eventually diagnosed with SCI. The mean MRS score at presentation was 1, at 3 months it was 4, and at 1 year it was 4.
Conclusion: Although the overall incidence of SCI is low, it should be considered in patients presenting with acute progressive myelopathic symptoms, even in the absence of vascular risk factors. Factors such as patient demographics and MRI lesion characteristics—including lesion location and ADC correlation—can help differentiate acute demyelinating conditions from SCI. Additionally, a third diagnosis should be considered, beyond just TM and SCI, as not all strokes follow typical patterns, and clinical presentation can vary significantly among patients. Furthermore, recovery outcomes can differ widely, emphasizing the need for individualized patient management.
Methods and Material: Retrospective review of electronic medical records was done. Patients with discharge diagnosis of spinal stroke with DWI imaging evidence of infarction, challenging cases with positive DWI imaging but different pattern of clinical presentation and exam findings were included in the study. Cases without spinal DWI imaging were excluded.
Results: Among the 34 DWI-positive patients included in the study with suspected SCI, the average age at presentation was 60 years, and 22 patients (64.7%) had vascular risk factors. A rapid onset of severe deficits, reaching their peak within 12 hours, was observed in 14 patients (41.1%), while 20 patients (58.8%) experienced a gradual decline. Sensory involvement was noted in 26 patients (76.4%), with 13 of these patients (50%) selectively retaining vibration and proprioception. Out of the 34 suspected SCI cases, 15 patients (44.1%) initially received alternative diagnoses, such as TM, NMOSD, Metastatic disease, Post-traumatic cord injury, or Post-laminectomy syndrome. However, after repeated imaging and continuous outpatient follow-up, 7 patients (46.6%) were eventually diagnosed with SCI. The mean MRS score at presentation was 1, at 3 months it was 4, and at 1 year it was 4.
Conclusion: Although the overall incidence of SCI is low, it should be considered in patients presenting with acute progressive myelopathic symptoms, even in the absence of vascular risk factors. Factors such as patient demographics and MRI lesion characteristics—including lesion location and ADC correlation—can help differentiate acute demyelinating conditions from SCI. Additionally, a third diagnosis should be considered, beyond just TM and SCI, as not all strokes follow typical patterns, and clinical presentation can vary significantly among patients. Furthermore, recovery outcomes can differ widely, emphasizing the need for individualized patient management.
More abstracts on this topic:
Intravenous Administration of Muse Cells Promotes Long-Lasting Functional Recovery in a Rat Model of Spinal Cord Ischemic Injury
Otani Masayuki, Saiki Yoshikatsu, Kushida Yoshihiro, Kuroda Yasumasa, Wakao Shohei, Abe Kana, Oguma Yo, Katahira Shintaro, Hosoyama Katsuhiro, Dezawa Mari
Biologic mechanisms of Early Exercise After Acute Ischemic Stroke and Intracerebral Hemorrhage (BEACH): A Pilot Randomized Controlled Trial of Cycle Ergometry after StrokeZink Elizabeth, Bahouth Mona, Ziai Wendy, Budhathoki Chakra
Readers' Comments
We encourage you to enter the discussion by posting your comments and questions below.
Presenters will be notified of your post so that they can respond as appropriate.
This discussion platform is provided to foster engagement, and simulate conversation and knowledge sharing.
You have to be authorized to post a comment. Please, Login or Signup.
Rate this abstract
(Maximum characters: 500)