Final ID:
A Case of Primary CNS Vasculitis Presenting as Intraparenchymal Hemorrhage in a Patient with Sickle Cell Trait
Case Summary: In less than 400 words, please summarize the case. Briefly describe the case and any particular complexities and/or complications encountered.: Primary CNS vasculitis (PCNSV) is a challenging diagnosis, often associated with connective tissue diseases or infections, but rarely presents initially with hemorrhage. While cerebral vasculopathy is documented in sickle cell anemia, it is uncommon in sickle cell trait. Sickle cell trait, however, is linked to microvascular occlusions and endothelial dysfunction, which may exacerbate inflammation in cerebral vessels, increasing the risk of hemorrhage. This case represents a rare presentation of CNS vasculitis manifesting as hemorrhage in a patient with sickle cell trait.
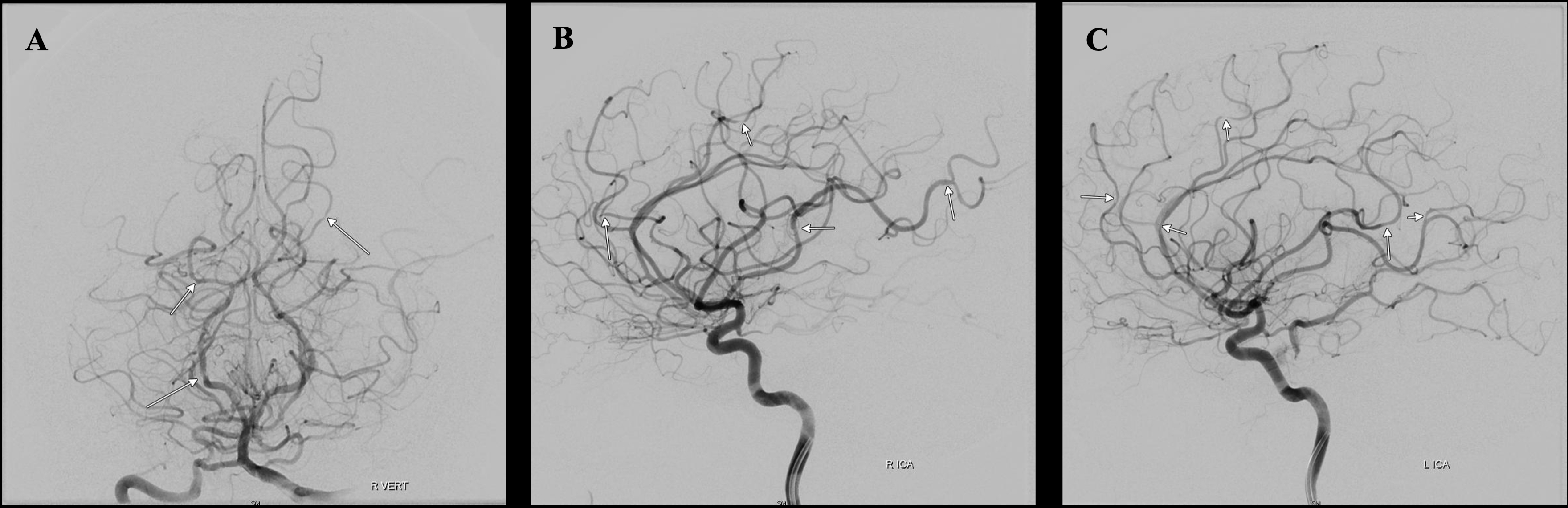
The patient is a 45-year-old female with a history of diabetes, hypertension, and sickle cell trait who presented with two months of headache and blurred vision which progressed to lethargy and confusion. CT revealed a left basal ganglia hemorrhage with intraventricular extension, initially attributed to hypertension given systolic blood pressure > 240 on admission. Scattered ischemic strokes were then noted on MRI. Conventional angiography demonstrated multiple areas of medium and small vessel narrowing, unresponsive to intra-arterial verapamil, consistent with vasculitis.
Cerebrospinal fluid (CSF) analysis showed elevated protein (177 mg/dL) and white blood cells (217 cell/uL) with negative cryptococcal antigen, syphilis antibodies, VZV, HHV6, HSF, and parvovirus B19. Flow cytometry was without evidence of lymphoma. Extensive infectious and autoimmune work up, including meningoecephalitis panels, myositis extended panel, ANA multiplex panel, complement levels, cryoglobulins, and common neurotrophic viruses were negative. Inflammatory markers ESR and CRP were markedly elevated at 120 and 62.66 respectively. Antiphospholipid antibodies and hypercoagulable work up were negative. Additional extracranial imaging showed no signs of systemic vasculitis.
The patient had repeat brain imaging due to worsened mental status which showed new infarcts in the bilateral ACA and MCA territories. Given the clinical suspicion for PCNSV, a brain biopsy was done. It revealed perivascular lymphocytic infiltration without other definitive pathologic changes. Despite the lack of conclusive biopsy findings, the patient was diagnosed with angiography-proven PCNSV. She had significant clinical improvement with high-dose corticosteroids and cyclophosphamide.
This case underscores the diagnostic complexity of PCNSV, especially in conditions such as sickle cell trait which may contribute to disease pathogenesis.
The patient is a 45-year-old female with a history of diabetes, hypertension, and sickle cell trait who presented with two months of headache and blurred vision which progressed to lethargy and confusion. CT revealed a left basal ganglia hemorrhage with intraventricular extension, initially attributed to hypertension given systolic blood pressure > 240 on admission. Scattered ischemic strokes were then noted on MRI. Conventional angiography demonstrated multiple areas of medium and small vessel narrowing, unresponsive to intra-arterial verapamil, consistent with vasculitis.
Cerebrospinal fluid (CSF) analysis showed elevated protein (177 mg/dL) and white blood cells (217 cell/uL) with negative cryptococcal antigen, syphilis antibodies, VZV, HHV6, HSF, and parvovirus B19. Flow cytometry was without evidence of lymphoma. Extensive infectious and autoimmune work up, including meningoecephalitis panels, myositis extended panel, ANA multiplex panel, complement levels, cryoglobulins, and common neurotrophic viruses were negative. Inflammatory markers ESR and CRP were markedly elevated at 120 and 62.66 respectively. Antiphospholipid antibodies and hypercoagulable work up were negative. Additional extracranial imaging showed no signs of systemic vasculitis.
The patient had repeat brain imaging due to worsened mental status which showed new infarcts in the bilateral ACA and MCA territories. Given the clinical suspicion for PCNSV, a brain biopsy was done. It revealed perivascular lymphocytic infiltration without other definitive pathologic changes. Despite the lack of conclusive biopsy findings, the patient was diagnosed with angiography-proven PCNSV. She had significant clinical improvement with high-dose corticosteroids and cyclophosphamide.
This case underscores the diagnostic complexity of PCNSV, especially in conditions such as sickle cell trait which may contribute to disease pathogenesis.
More abstracts on this topic:
Readers' Comments
We encourage you to enter the discussion by posting your comments and questions below.
Presenters will be notified of your post so that they can respond as appropriate.
This discussion platform is provided to foster engagement, and simulate conversation and knowledge sharing.
You have to be authorized to post a comment. Please, Login or Signup.
Rate this abstract
(Maximum characters: 500)