Final ID: TP247
Iatrogenic Cervical Artery Dissections during Endovascular Interventions
Abstract Body: Introduction:
Iatrogenic cervical artery dissection (CeAD) may result from various procedures such as procedural and diagnostic angiography. Due to the rarity of iatrogenic CeAD, existing literature on management and outcomes is limited. This observational cohort study investigates clinical approaches and long-term outcomes of iatrogenic CeAD after endovascular interventions.
Methods:
We conducted a retrospective chart review to analyze patients who underwent endovascular treatments at the Mayo Clinic from 1998 to 2021. We focused on patients with iatrogenic CeAD resulting from interventions. Pertinent patient factors were extracted. Descriptive statistics highlighted the relationship between treatments and long-term clinical outcomes.
Results:
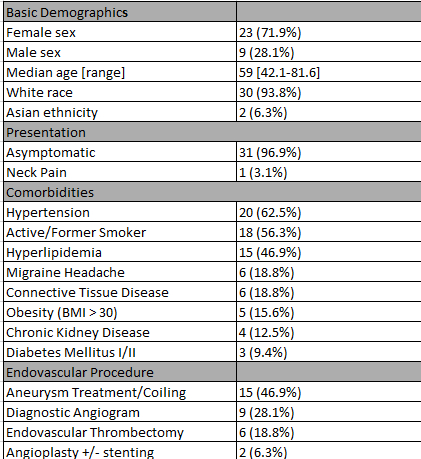
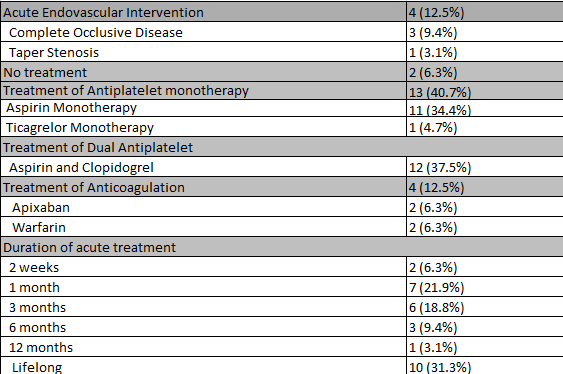
Between 1998 and 2021, 21,191 patients underwent catheter cerebral angiography. Among them, 32 had iatrogenic CeAD (30 identified as white, 23 women, median age 59 [range 40.5–92.9]). Common comorbidities included hypertension (62.5%), smoking (56.3%), and hyperlipidemia (46.9%). Of the 32 patients, 9(28.1%) had dissection with diagnostic angiograms, 6(18.8%) endovascular thrombectomy, 15(46.9%) aneurysm treatment, and 2(6.3%) angioplasty with or without stenting. The location of dissections was dependent upon the intervention: 17(53.1%) had internal carotid artery dissection, 13(40.6%) vertebral artery dissection, and 2(6.3%) common carotid dissection. One patient was symptomatic with neck pain. All dissections were diagnosed by cerebral angiography during the same session as the initial intervention. Only 4(12.5%) were treated with hyperacute stenting. Following diagnosis, 30(93.7%) were placed on antithrombotic therapy, including aspirin alone (34.4%) or dual antiplatelet therapy with aspirin and clopidogrel (37.5%). The median duration of acute treatment was 3 months. The median duration of imaging follow up was 1022 days. Follow-up imaging showed an excellent radiological course, with complete or nearly complete dissection remodeling.
Conclusions:
Iatrogenic CeAD with endovascular interventions is rare and typically benign. Most cases are managed medically without significant clinical complications or long-term negative outcomes. Single or dual antiplatelet therapies remain preferred treatments, in line with current trends. Key factors influencing clinical decision-making include location, occlusion rate, pseudoaneurysm formation, intracranial extension, distal collateral circulation, and ischemia.
Iatrogenic cervical artery dissection (CeAD) may result from various procedures such as procedural and diagnostic angiography. Due to the rarity of iatrogenic CeAD, existing literature on management and outcomes is limited. This observational cohort study investigates clinical approaches and long-term outcomes of iatrogenic CeAD after endovascular interventions.
Methods:
We conducted a retrospective chart review to analyze patients who underwent endovascular treatments at the Mayo Clinic from 1998 to 2021. We focused on patients with iatrogenic CeAD resulting from interventions. Pertinent patient factors were extracted. Descriptive statistics highlighted the relationship between treatments and long-term clinical outcomes.
Results:
Between 1998 and 2021, 21,191 patients underwent catheter cerebral angiography. Among them, 32 had iatrogenic CeAD (30 identified as white, 23 women, median age 59 [range 40.5–92.9]). Common comorbidities included hypertension (62.5%), smoking (56.3%), and hyperlipidemia (46.9%). Of the 32 patients, 9(28.1%) had dissection with diagnostic angiograms, 6(18.8%) endovascular thrombectomy, 15(46.9%) aneurysm treatment, and 2(6.3%) angioplasty with or without stenting. The location of dissections was dependent upon the intervention: 17(53.1%) had internal carotid artery dissection, 13(40.6%) vertebral artery dissection, and 2(6.3%) common carotid dissection. One patient was symptomatic with neck pain. All dissections were diagnosed by cerebral angiography during the same session as the initial intervention. Only 4(12.5%) were treated with hyperacute stenting. Following diagnosis, 30(93.7%) were placed on antithrombotic therapy, including aspirin alone (34.4%) or dual antiplatelet therapy with aspirin and clopidogrel (37.5%). The median duration of acute treatment was 3 months. The median duration of imaging follow up was 1022 days. Follow-up imaging showed an excellent radiological course, with complete or nearly complete dissection remodeling.
Conclusions:
Iatrogenic CeAD with endovascular interventions is rare and typically benign. Most cases are managed medically without significant clinical complications or long-term negative outcomes. Single or dual antiplatelet therapies remain preferred treatments, in line with current trends. Key factors influencing clinical decision-making include location, occlusion rate, pseudoaneurysm formation, intracranial extension, distal collateral circulation, and ischemia.
More abstracts on this topic:
Ascending Thoracic Aortic Aneurysms in a Veterans Affairs Health System: Longitudinal Outcomes and Risk Factors
Gomez Axel, Carroway William, Ge Liang, Boskovski Marko, Tseng Elaine
Adipocyte TRPM7 promotes aortic dissection by accelerating SMC phenotype switchingWang Mi, Gao Min
Readers' Comments
We encourage you to enter the discussion by posting your comments and questions below.
Presenters will be notified of your post so that they can respond as appropriate.
This discussion platform is provided to foster engagement, and simulate conversation and knowledge sharing.
You have to be authorized to post a comment. Please, Login or Signup.
Rate this abstract
(Maximum characters: 500)