Final ID: TP261
Stroke in pediatric heart transplant patients
Methods: Retrospective cohort study of consecutive PHT Pts at a tertiary center between 09/01/2012 and 09/30/2022. Demographic, and pre-, intra-, and post-PHT clinical, brain imaging and RT (physical, occupational, speech and feeding therapy) data were collected up to PHT hospitalization. Data are presented as frequency (%) or median (Inter Quartile Range-IQR).
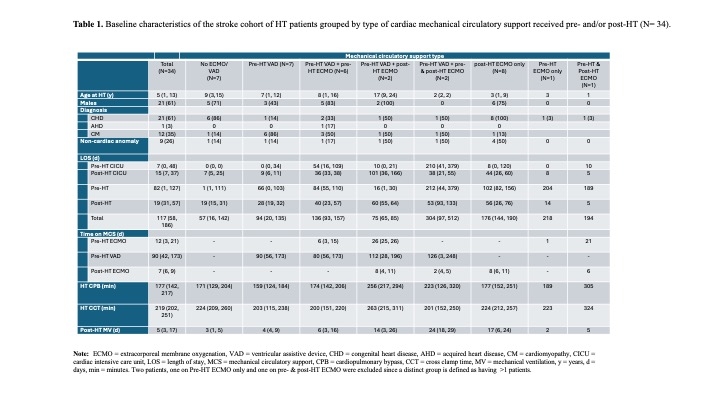
Results: Of the 83 PHT Pts 34(40%) of them had a stroke 20(59%) pre-PHT, 7(21%) post-PHT, 4(12%) pre- and post-PHT and unknown timing in 3(9%). Median age of HT in these Pts was 6 yrs(1,13) (Table 1), 21(62%) were male. CHD was the pre-PHT diagnosis in 21(62%) of stroke Pts, cardiomyopathy in 12(35%) and acquired heart disease in 1(3%). Mechanical circulatory support were used in 27(79%) PHT with stroke.
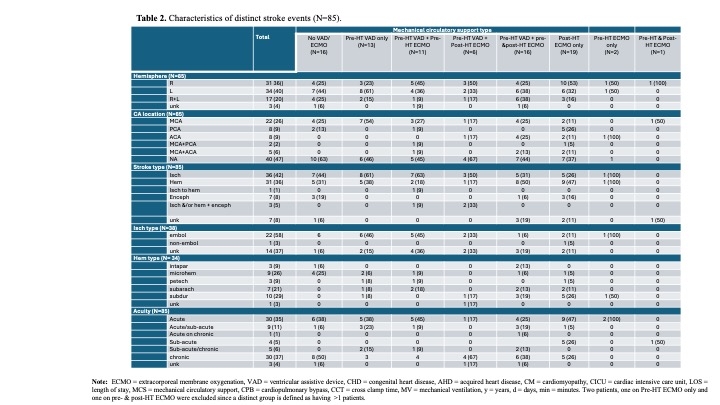
Total no. of distinct areas of neurologic injury on brain MRI was 85 (Table 2). Neurologic events per imaging were 2(1, 2). MCA was affected in 22(26%), PCA 8(9%), ACA 8(9%), MCA+ACA 5(6%), and MCA+PCA 2(2%). Additionally, 38(45%) were ischemic and 34(40%) were hemorrhagic strokes.
Of the acute and/or sub-acute brain MRI findings with known stroke dates(N=41), the week prior, 8(20%) of Pts had a cardiac surgery, 4(10%) had a cardiac cath, 3(7%) had a cardiac arrest, 7(17%) had an arrest+procedure, 5(12%) arrest+cath, 3(7%) had a cath+ procedure, and 1(3%) had an arrest+cath+procedure.
Of the 41 brain MRI findings with known stroke dates, 1 day prior, 8(24%) pts were on anticoagulation agents, 10(24%) on antiplatelet, 15(37%) were on both, and 8(20%) were on neither. Pts who required ECMO and/or VAD(76%) had more strokes.
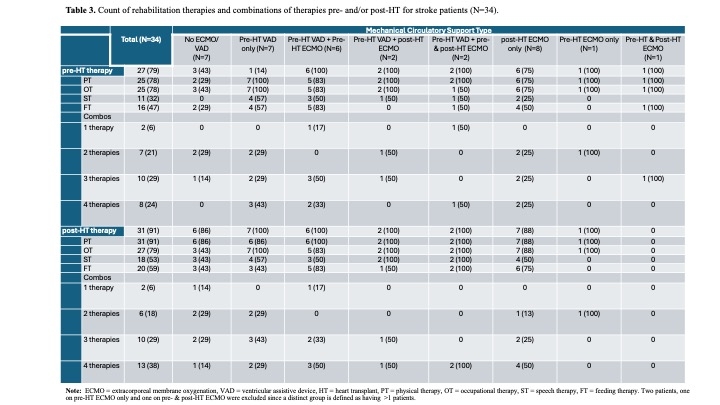
Total LOS for Pts with strokes was 91 days(28, 167) vs. the total HT cohort 117 days(58, 186). Of the stroke Pts, Pre-HT and Post-HT RT were required in 27(79%) and 31(91%), respectively (Table 3). Acute inpatient rehabilitation was required in 9(26%).
Conclusions: Strokes are found in almost half of PHT Pts. Most of them occur pre-HT. Cause of stroke is likely multifactorial. Their functional status is frequently impacted and requires RT pre- and post-HT.
More abstracts on this topic:
Thatte Nikhil, Del Nido Pedro, Ghelani Sunil, Hammer Peter, Marx Gerald, Beroukhim Rebecca, Gauvreau Kimberlee, Callahan Ryan, Prakash Ashwin, Emani Sitaram, Hoganson David
Assessing Racial Disparities in Heart Transplant Allocations Post-2018 Policy ChangeMalkani Kabir, Zhang Ruina, Li Han, Ezema Ashley, Steitieh Diala, Purkayastha Subhanik, Kini Vinay
Readers' Comments
We encourage you to enter the discussion by posting your comments and questions below.
Presenters will be notified of your post so that they can respond as appropriate.
This discussion platform is provided to foster engagement, and simulate conversation and knowledge sharing.
You have to be authorized to post a comment. Please, Login or Signup.