Final ID: TMP15
Stroke Nurse Navigator Structured Phone Call Protocol to Improve Transitions of Care After Stroke
Abstract Body: Background: After discharge can be a vulnerable time for stroke patients and their caregivers. Nurse navigators have been utilized in other specialties resulting in positive impacts on patient care. Nurse navigators are becoming an important part of Stroke Center teams. Responsibilities vary, including patient education and post-discharge phone calls. A Primary Stroke Center found nurse navigator post-discharge calls improved follow-up and decreased 30-day stroke and all cause readmissions.
Purpose: To implement a Stroke Nurse Navigator (SNN) at a Comprehensive Stroke Center (CSC), providing in-person stroke education during the hospitalization and a structured post-discharge phone call protocol with the patient and/or caregiver. The goal is to connect care settings, improve transitions of care, improve secondary stroke prevention medication adherence, and increase Stroke Clinic follow-up.
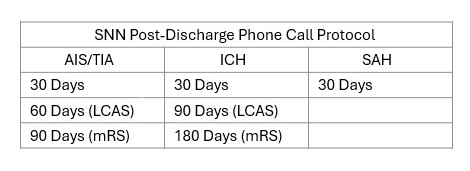
Methods: All patients discharged with stroke, including TIA, AIS, ICH, and SAH receive post-discharge phone calls by the SNN. Additional high risk patients can be added at discretion. Patients discharged home receive a call within 7 post-discharge in which the SNN reviews and verifies the patient’s Stroke Clinic follow-up, outpatient testing, and medications. Stroke symptom recognition and patient concerns are also discussed. All patients regardless of discharge disposition receive calls at various time points post-discharge. The call time points were determined based on predictive recovery curves for stroke subtypes and to anticipate potential vulnerable points after discharge; e.g. AIS patients receive calls at 30, 60, and 90 days post-discharge. For the 30 day call, the SNN reviews the patient’s stroke risk factors and educates on interventions. A Late Complications After Stroke (LCAS) screening tool to identify complications, like depression and headaches is completed at the 60/90 day call. Concerns are communicated to the outpatient stroke clinician to address at follow-up. During the 90/180 day call, a mRS is completed. Calls are completed with the patient or caregiver if the patient is unable to participate for any reason.
Discussion: The impact of a structured post-discharge call protocol on secondary stroke prevention medication adherence and Stroke Clinic retention will be evaluated. This initiative aims to prove that it is feasible and beneficial to have a SNN and post-discharge calls as standard of care for stroke patients to improve transitions of care.
Purpose: To implement a Stroke Nurse Navigator (SNN) at a Comprehensive Stroke Center (CSC), providing in-person stroke education during the hospitalization and a structured post-discharge phone call protocol with the patient and/or caregiver. The goal is to connect care settings, improve transitions of care, improve secondary stroke prevention medication adherence, and increase Stroke Clinic follow-up.
Methods: All patients discharged with stroke, including TIA, AIS, ICH, and SAH receive post-discharge phone calls by the SNN. Additional high risk patients can be added at discretion. Patients discharged home receive a call within 7 post-discharge in which the SNN reviews and verifies the patient’s Stroke Clinic follow-up, outpatient testing, and medications. Stroke symptom recognition and patient concerns are also discussed. All patients regardless of discharge disposition receive calls at various time points post-discharge. The call time points were determined based on predictive recovery curves for stroke subtypes and to anticipate potential vulnerable points after discharge; e.g. AIS patients receive calls at 30, 60, and 90 days post-discharge. For the 30 day call, the SNN reviews the patient’s stroke risk factors and educates on interventions. A Late Complications After Stroke (LCAS) screening tool to identify complications, like depression and headaches is completed at the 60/90 day call. Concerns are communicated to the outpatient stroke clinician to address at follow-up. During the 90/180 day call, a mRS is completed. Calls are completed with the patient or caregiver if the patient is unable to participate for any reason.
Discussion: The impact of a structured post-discharge call protocol on secondary stroke prevention medication adherence and Stroke Clinic retention will be evaluated. This initiative aims to prove that it is feasible and beneficial to have a SNN and post-discharge calls as standard of care for stroke patients to improve transitions of care.
More abstracts on this topic:
A Simple One-Item Nursing Falls Assessment Predicts Outcomes For Patients With Stage D Heart Failure Undergoing Surgical Advanced Therapies
Salvador Vincent, Perez Jaime Abraham, Hudec Paige, Gorodeski Eiran, Oneill Thomas
A Trial of Patients Receiving Remote Ischemic Conditioning in Early Stroke (PRICES) in a Tertiary Hospital in the Philippines: An Open Label StudyAng Kevin Royce, Juangco Dan, Hernandez Maria Kim
Readers' Comments
We encourage you to enter the discussion by posting your comments and questions below.
Presenters will be notified of your post so that they can respond as appropriate.
This discussion platform is provided to foster engagement, and simulate conversation and knowledge sharing.
You have to be authorized to post a comment. Please, Login or Signup.
Rate this abstract
(Maximum characters: 500)