Final ID: 109
Geographical Trends in Cerebrovascular Disease Mortality in the United States, 1999-2020
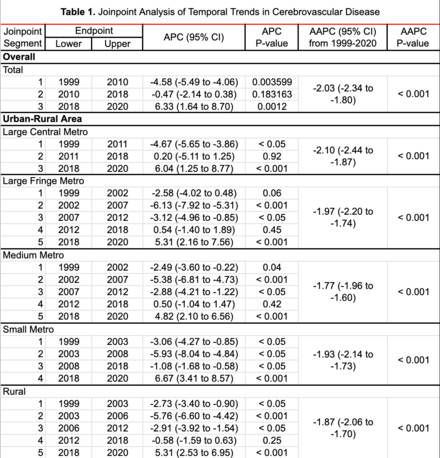
Methods: This retrospective cohort study analyzed 5,387,782 death certificates from 1999 to 2020, obtained from the CDC Wide-ranging Online Data for Epidemiologic Research (WONDER) database, focusing on cerebrovascular disease, defined by ICD-10 codes I60-I69. Age-adjusted mortality rates (AAMRs) per 100,000 were calculated based on the 2000 U.S. standard population. Temporal trends in mortality rates, stratified by urban-rural classification (large central metro, large fringe metro, medium metro, small metro, rural) and state, were characterized using the Joinpoint Regression Program, version 5.2.0 (National Cancer Institute). Statistical analyses were performed using RStudio 4.4.1, with p < 0.05 indicating significance. This study used deidentified, publicly available data and was deemed not human research by the University of Nevada, Reno IRB.
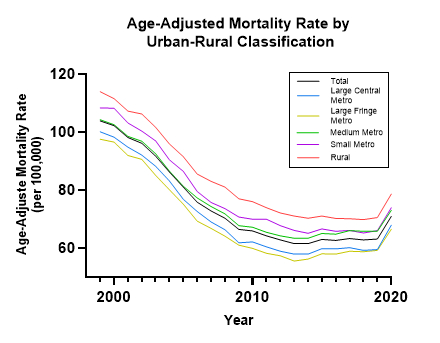
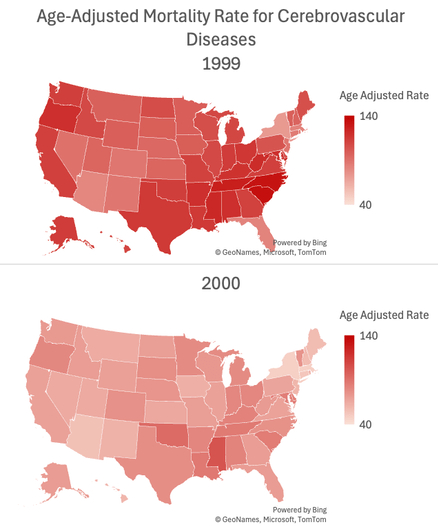
Results: From 1999 to 2020, the overall U.S. AAMR for cerebrovascular disease declined, with an average annual percent change (AAPC) of -2.03% (95% CI: -2.34 to -1.80, p < 0.001). Rural areas consistently had the highest AAMRs throughout the 22-year study period, though they decreased from 113.9 per 100,000 in 1999 to 78.6 in 2020. A significant upward trend was observed from 2018 onwards across all urban-rural classifications, with rural areas experiencing a 5.31% (95% CI: 2.53 to 6.95, p < 0.001) increase in AAMR between 2018 and 2020. State-level analysis showed significant variability among states, with states like Mississippi having persistently high AAMRs, despite overall declines.
Conclusion: This study highlights a significant overall decline in U.S. cerebrovascular disease mortality from 1999 to 2020, alongside a recent concerning increase beginning in 2018, particularly in rural areas and certain states. These findings underscore the need for targeted public health interventions to address emerging disparities in cerebrovascular disease outcomes by region and urbanization level.
More abstracts on this topic:
Wong Ka-ho, Krothapalli Neeharika, Littig Lauren, Champagne Alison, Majersik Jennifer, Reddy Vivek, De Havenon Adam
Burden of Chronic Kidney Disease Due to Hypertension Attributable to Dietary Risk Factors: Global Trends and Regional Inequities (1990–2021)Dudhat Kushal, Patel Ridham, Patel Juhi, Desai Hardik, Amin Vishrant, Patel Vishva, Zinzala Hardik, Patel Ker, Sakariya Dhrumil Chhaganbhai, Patel Kevin, Patel Kesar, Gopi Gokul, Sami Shahzad Ahmed
Readers' Comments
We encourage you to enter the discussion by posting your comments and questions below.
Presenters will be notified of your post so that they can respond as appropriate.
This discussion platform is provided to foster engagement, and simulate conversation and knowledge sharing.
You have to be authorized to post a comment. Please, Login or Signup.