Final ID: WP16
ROLE OF EPTIFIBATIDE IN POST-THROMBECTOMY STENOSIS
Abstract Body: INTRODUCTION
Currently, no level A evidence exists for the optimal rescue strategy for cases at high risk for re-occlusion following endovascular thrombectomy (EVT) in acute ischemic stroke. Glycoprotein IIb/IIIa inhibitors, which inhibit platelet aggregation and adhesion, show promise as adjunctive therapy, potentially yielding favorable outcomes, especially in residual stenosis cases.
METHODS
In this retrospective review study, we included patients aged ≥18 who underwent EVT at a comprehensive stroke center with TICI 2b or 2c outcome (admitted between 2019 – 2024), who were noted to have high-risk residual stenosis on angiography after EVT. We defined high-risk post-EVT stenosis as any stenosis with ≥50% lumen stenosis, associated dissection, re-occlusion during thrombectomy, and severe residual luminal irregularity. We excluded patients who had a clear contraindication to Eptifibatide, received a stent, or if the luminal stenosis was related to reactive vasospasm and any cases with TICI 0, 1, or TICI 3 scores.
RESULTS
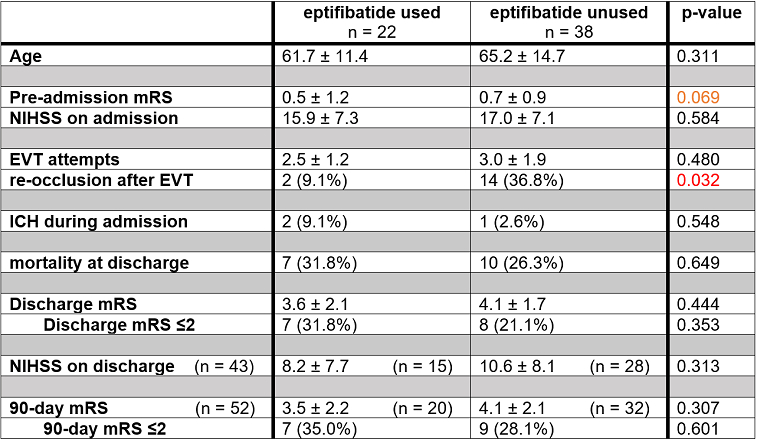
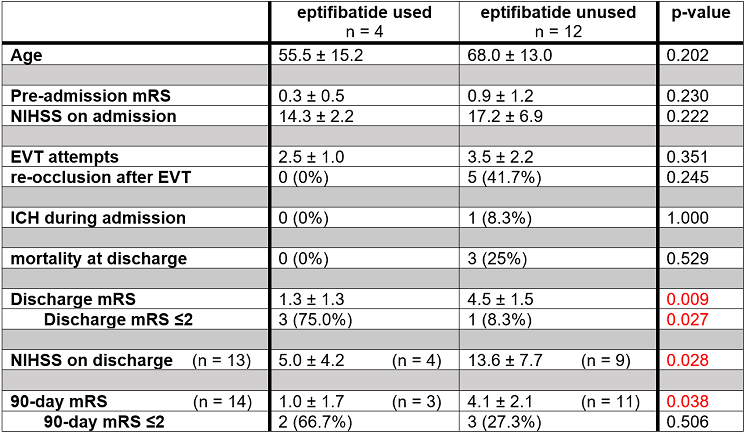
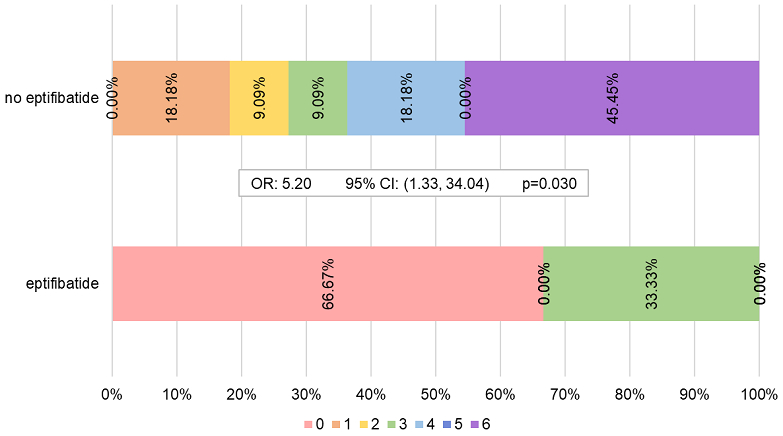
Our sample size was 60 (51.7% male, 48.3% female, mean age 63.9). Mean National Institute of Health Stroke Scale (NIHSS) on admission was 16.6; 36.7% (n=22) received eptifibatide. The rate of re-occlusion was significantly lower in patients who received eptifibatide compared to those who did not (9.1% vs. 36.8%, p=0.032). There was no difference in pre-stroke modified Rankin scale (mRS), NIHSS on admission, mortality, discharge mRS, or 90-day mRS between these two groups, nor between patients who received intravenous thrombolysis (IVT) vs. those who did not. However, among the 16 patients who received IVT, those who also received eptifibatide had significantly lower mean discharge NIHSS (5.0 vs. 13.6, p=0.028), discharge mRS (1.3 vs. 4.5, p=0.009), and 90-day mRS (1.0 vs. 4.1, p=0.038) than those who did not. Ordinal logistic regression of discharge mRS and 90-day mRS in IVT recipients with vs. without eptifibatide usage also revealed significant odds of lower mRS at both timepoints with eptifibatide (OR 7.23, p=0.011 and OR 5.2, p=0.030 respectively).
CONCLUSIONS
Eptifibatide use is associated with lower re-occlusion rates in patients with residual high-risk stenosis after EVT. Among IVT recipients with post-EVT residual stenosis, eptifibatide use is associated with improved discharge mRS, discharge NIHSS, and 90-day mRS. Given our limited sample size, these findings need to be evaluated further with larger Randomized Control Trials.
Currently, no level A evidence exists for the optimal rescue strategy for cases at high risk for re-occlusion following endovascular thrombectomy (EVT) in acute ischemic stroke. Glycoprotein IIb/IIIa inhibitors, which inhibit platelet aggregation and adhesion, show promise as adjunctive therapy, potentially yielding favorable outcomes, especially in residual stenosis cases.
METHODS
In this retrospective review study, we included patients aged ≥18 who underwent EVT at a comprehensive stroke center with TICI 2b or 2c outcome (admitted between 2019 – 2024), who were noted to have high-risk residual stenosis on angiography after EVT. We defined high-risk post-EVT stenosis as any stenosis with ≥50% lumen stenosis, associated dissection, re-occlusion during thrombectomy, and severe residual luminal irregularity. We excluded patients who had a clear contraindication to Eptifibatide, received a stent, or if the luminal stenosis was related to reactive vasospasm and any cases with TICI 0, 1, or TICI 3 scores.
RESULTS
Our sample size was 60 (51.7% male, 48.3% female, mean age 63.9). Mean National Institute of Health Stroke Scale (NIHSS) on admission was 16.6; 36.7% (n=22) received eptifibatide. The rate of re-occlusion was significantly lower in patients who received eptifibatide compared to those who did not (9.1% vs. 36.8%, p=0.032). There was no difference in pre-stroke modified Rankin scale (mRS), NIHSS on admission, mortality, discharge mRS, or 90-day mRS between these two groups, nor between patients who received intravenous thrombolysis (IVT) vs. those who did not. However, among the 16 patients who received IVT, those who also received eptifibatide had significantly lower mean discharge NIHSS (5.0 vs. 13.6, p=0.028), discharge mRS (1.3 vs. 4.5, p=0.009), and 90-day mRS (1.0 vs. 4.1, p=0.038) than those who did not. Ordinal logistic regression of discharge mRS and 90-day mRS in IVT recipients with vs. without eptifibatide usage also revealed significant odds of lower mRS at both timepoints with eptifibatide (OR 7.23, p=0.011 and OR 5.2, p=0.030 respectively).
CONCLUSIONS
Eptifibatide use is associated with lower re-occlusion rates in patients with residual high-risk stenosis after EVT. Among IVT recipients with post-EVT residual stenosis, eptifibatide use is associated with improved discharge mRS, discharge NIHSS, and 90-day mRS. Given our limited sample size, these findings need to be evaluated further with larger Randomized Control Trials.
More abstracts on this topic:
A Polypill Strategy for Lipid Lowering and Anti-Platelet Therapy After Acute Coronary Syndrome: A Pilot Randomized Controlled Trial
Keshvani Neil, Wang Thomas, Pandey Ambarish, Coellar Juan David, Rizvi Syed Kazim, Jain Anand, Bustillo-rubio M. Karina, Segar Matthew, Lokesh Nidhish, Miller James, Yates Sean
A Fecal-Derived Commensal Bacterium BM109 Reduces Infarct Size and Neurological Deficits in an Ischemic Stroke Rat ModelYoon Chung Eun, Kim You Bin, Nam Hyo Suk
Readers' Comments
We encourage you to enter the discussion by posting your comments and questions below.
Presenters will be notified of your post so that they can respond as appropriate.
This discussion platform is provided to foster engagement, and simulate conversation and knowledge sharing.
You have to be authorized to post a comment. Please, Login or Signup.
Rate this abstract
(Maximum characters: 500)