Final ID: WP209
Comparative Functional Outcomes for Ischemic Stroke Patients with and without COVID-19
Abstract Body: Background: COVID-19, primarily a respiratory illness caused by SARS-CoV-2, is associated with vascular complications like ischemia due to endothelial injury, hypercoagulability, and inflammation. This study examines how COVID-19 affects functional outcomes of ischemic stroke patients.
Methods: Ischemic stroke patients admitted to our Joint Commission-certified primary stroke center were retrospectively analyzed from March 1, 2020, to March 1, 2022. A subgroup analysis was conducted for patients during the vaccination period (April 14, 2021, to March 1, 2022). Patients were included if they were ≥18 years old and had a stroke on admission or during hospitalization. Univariate and multivariable analyses were used, with a significance threshold of p<0.05.
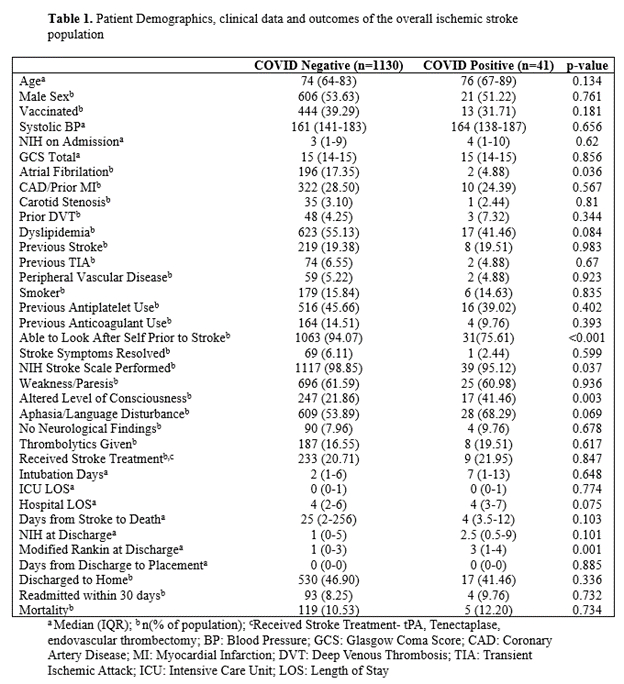
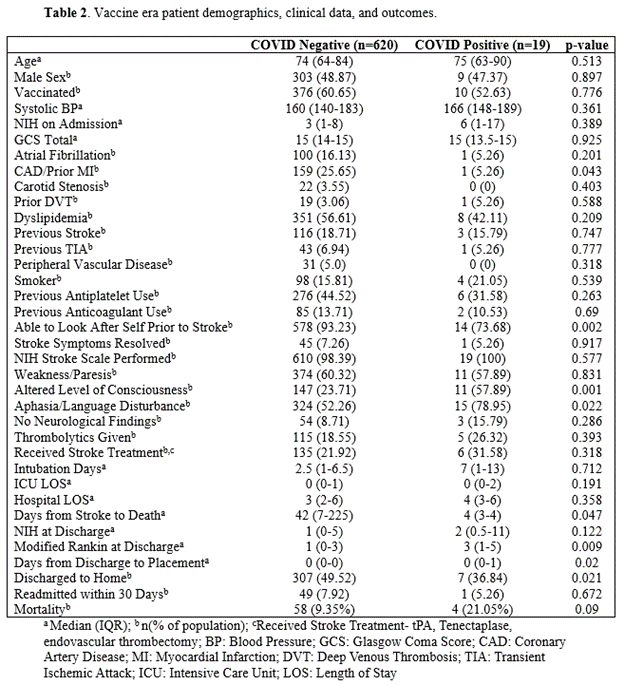
Results: Out of 1,171 patients, those who tested positive for COVID-19 had significantly worse outcomes. Demographics, clinical data, and outcomes are found in Table 1. COVID-19 Positive patients experienced fewer days between stroke and death (4 days vs. 25 days, p=0.047), higher modified Rankin Scale (mRS) scores at discharge (3 vs. 1, p=0.001), and increased rates of altered consciousness (41.46% vs. 21.86%, p=0.03). In the vaccination period subgroup, COVID-positive patients had fewer days from stroke to death (4 days vs. 42 days, p=0.047), worse mRS scores (3 vs. 1, p=0.009), longer delays in discharge placement (0 vs. 1 day, p=0.020), and higher rates of altered consciousness (57.89% vs. 23.71%, p=0.001). Additionally, COVID-negative patients were more likely to be discharged home (49.52% vs. 36.84%, p=0.021). Multivariable analysis identified higher NIHSS at admission (OR: 1.028 [1.003–1.053], p=0.027), older age (OR: 1.027 [1.011–1.045], p=0.001), and a history of diabetes (OR: 1.596 [1.056–2.413], p=0.027) as increased mortality risks.
Conclusion: COVID-19 is associated with worse recovery outcomes and discharge delays for ischemic stroke patients compared to those without COVID-19. Further research is needed to explore these differences and their implications for stroke management amid the ongoing global health crisis.
Methods: Ischemic stroke patients admitted to our Joint Commission-certified primary stroke center were retrospectively analyzed from March 1, 2020, to March 1, 2022. A subgroup analysis was conducted for patients during the vaccination period (April 14, 2021, to March 1, 2022). Patients were included if they were ≥18 years old and had a stroke on admission or during hospitalization. Univariate and multivariable analyses were used, with a significance threshold of p<0.05.
Results: Out of 1,171 patients, those who tested positive for COVID-19 had significantly worse outcomes. Demographics, clinical data, and outcomes are found in Table 1. COVID-19 Positive patients experienced fewer days between stroke and death (4 days vs. 25 days, p=0.047), higher modified Rankin Scale (mRS) scores at discharge (3 vs. 1, p=0.001), and increased rates of altered consciousness (41.46% vs. 21.86%, p=0.03). In the vaccination period subgroup, COVID-positive patients had fewer days from stroke to death (4 days vs. 42 days, p=0.047), worse mRS scores (3 vs. 1, p=0.009), longer delays in discharge placement (0 vs. 1 day, p=0.020), and higher rates of altered consciousness (57.89% vs. 23.71%, p=0.001). Additionally, COVID-negative patients were more likely to be discharged home (49.52% vs. 36.84%, p=0.021). Multivariable analysis identified higher NIHSS at admission (OR: 1.028 [1.003–1.053], p=0.027), older age (OR: 1.027 [1.011–1.045], p=0.001), and a history of diabetes (OR: 1.596 [1.056–2.413], p=0.027) as increased mortality risks.
Conclusion: COVID-19 is associated with worse recovery outcomes and discharge delays for ischemic stroke patients compared to those without COVID-19. Further research is needed to explore these differences and their implications for stroke management amid the ongoing global health crisis.
More abstracts on this topic:
A Trial of Patients Receiving Remote Ischemic Conditioning in Early Stroke (PRICES) in a Tertiary Hospital in the Philippines: An Open Label Study
Ang Kevin Royce, Juangco Dan, Hernandez Maria Kim
A Multi-centre, Randomized, Controlled Study of External CounterPulsation for Patients with Recent Atherosclerotic Stroke (SPA)Xiong Li, Chen Xiangyan, Leung Howan, Zhu Lixia, Leung Thomas, Wong Lawrence
Readers' Comments
We encourage you to enter the discussion by posting your comments and questions below.
Presenters will be notified of your post so that they can respond as appropriate.
This discussion platform is provided to foster engagement, and simulate conversation and knowledge sharing.
You have to be authorized to post a comment. Please, Login or Signup.
Rate this abstract
(Maximum characters: 500)