Final ID: WP172
Invariant Pupil Reactivity (PuRe) Score: Robust Smartphone-based Pupillometry for Critical Care Across Lighting, Measurement Conditions, and Hardware Variations
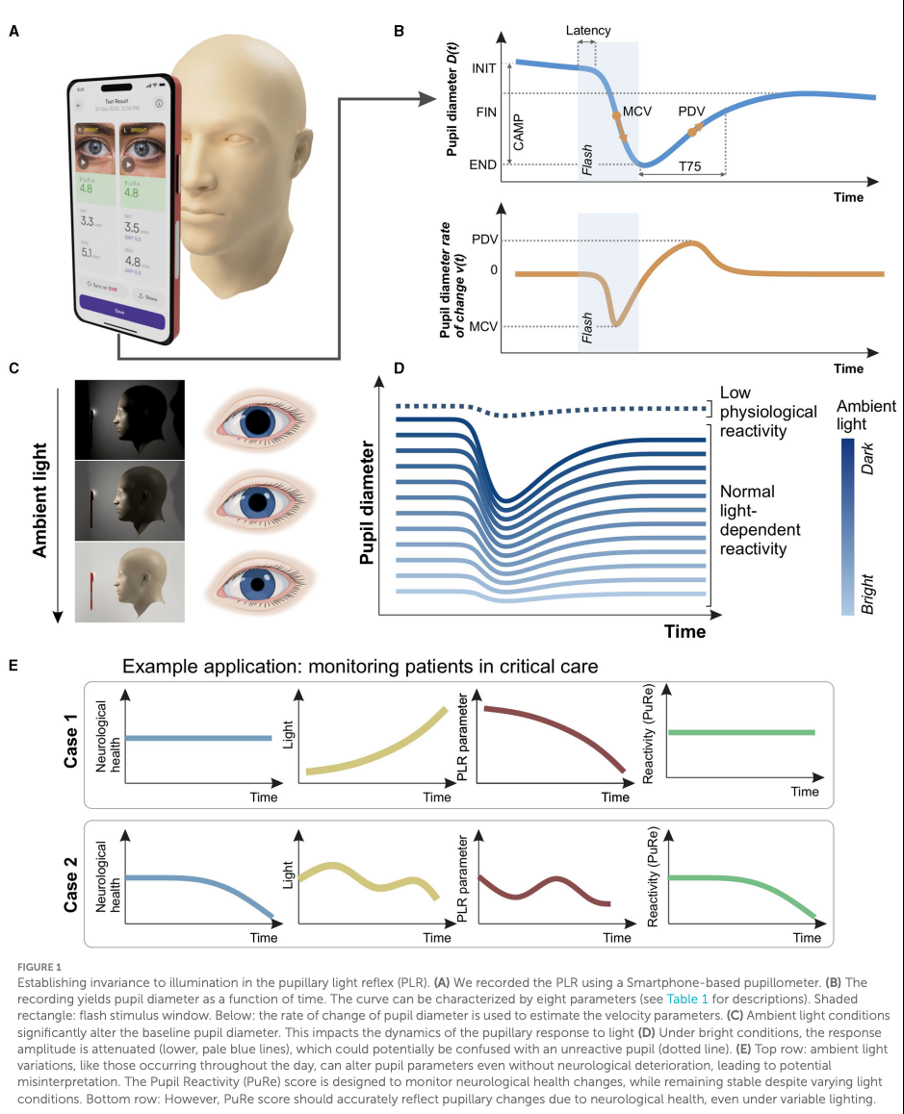
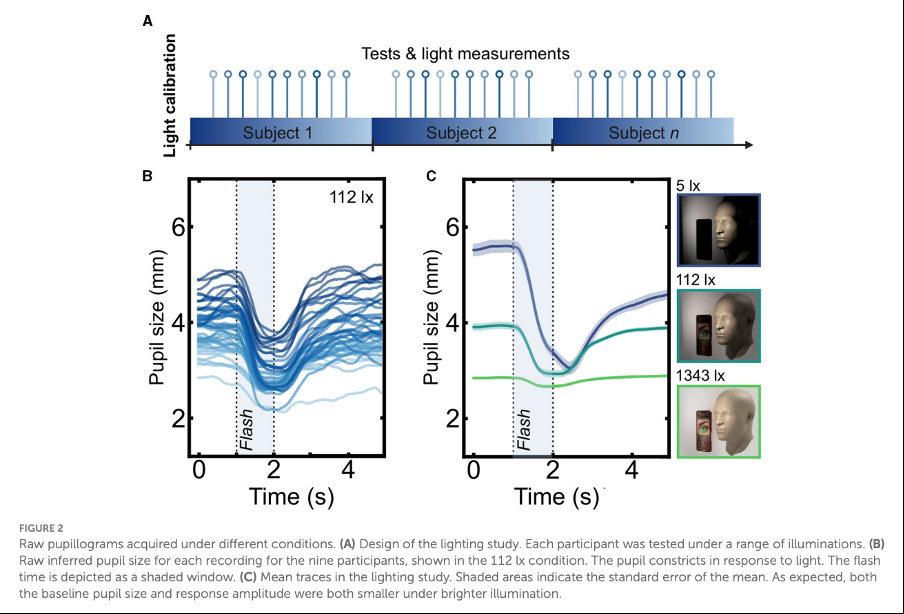
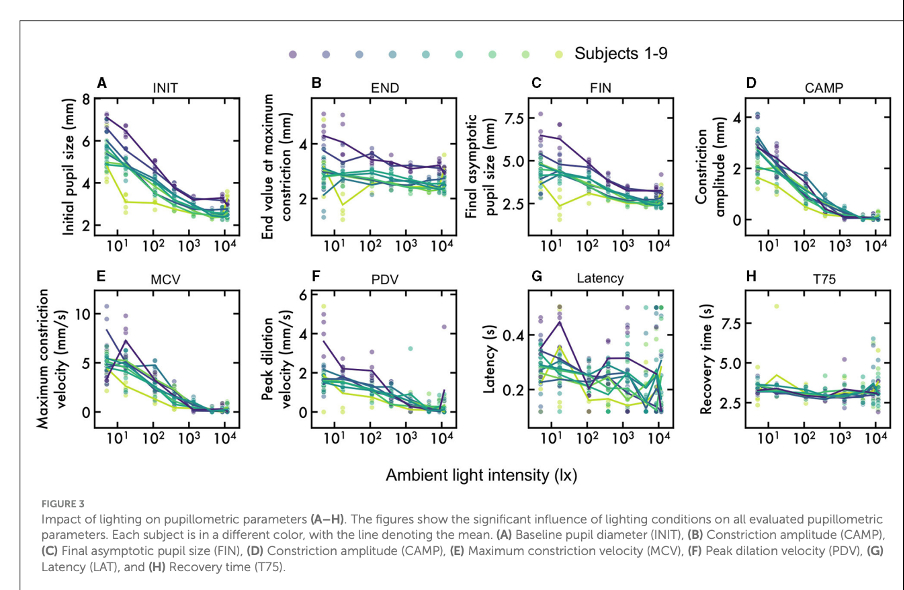
We conducted two studies to validate PuRe score stability. At Nicolaus Copernicus University (Ethics ref: KB42712021), we collected 309 recordings under various lighting conditions (5-11,800 lux). Additionally, we performed 300 measurements on 2 volunteers using three iPhone models (SE2, 13, 15Pro) at phone-face distances of 50-210 mm in dim lighting (275-350 lux). We developed adaptive algorithms to recognize the scene, adjust flash intensity, and provide real-time guidance for positioning. We compared measurements using fixed vs. adaptive settings.
The lighting study showed no significant correlation between pupil reactivity and illumination (Pearson's r=0.064, p=0.26). In the hardware/distance study, a linear mixed effects model showed that adaptive settings significantly reduced parameter dependence on distance: constriction amplitude (F(1,198)=9.27, p=0.0026), ratio (F(1,198)=11.02, p=0.0011), and PuRe score (F(1,198)=10.15, p=0.0017). Without adaptive settings, parameters varied significantly with distance (p<0.001), while adaptive settings eliminated these effects (p>0.5) with no significant device-related differences (F(2,99)=1.47, p=0.235).
The AI-powered pupillometer app with the invariant PuRe score shows consistent performance across varied lighting, distances, and phone models. This reliability enables effective pupillary assessment in diverse critical care and rehabilitation settings, promoting adoption for standardized neurological monitoring. The system's adaptability supports centralized health record data collection and consistent evaluation across care environments, regardless of measurement conditions or device models.
References:
Ong C, et al. (2019). Neurocrit Care, 30:316-321.
Bogucki A, et al. (2024). Front Neurol, 15:1363190. 10.3389/fneur.2024.1363190
Bogucki A, et al. (2024). i-Perception, 15(1):1-4.
More abstracts on this topic:
Vo Alexander, Rho Howard, Sangha Navi, Khrlobyan Manya, Han Seungyong, Modjtahedi Bobeck, Taleb Shayandokht, Cheng Pamela, Ajani Zahra, Le Duy, Ly An
A Machine Learning-Derived Socio-Environmental Risk Score More Accurately Predicts Cardiovascular Events and Better Addresses Health Inequities than Social Deprivation IndexChen Zhuo, Nasir Khurram, Al-kindi Sadeer, Rajagopalan Sanjay, Ponnana Sai Rahul, Dazard Jean-eudes, Zhang Tong, Dong Weichuan, Okyere Robert, Sirasapalli Santosh, Deo Salil, Khraishah Haitham
Readers' Comments
We encourage you to enter the discussion by posting your comments and questions below.
Presenters will be notified of your post so that they can respond as appropriate.
This discussion platform is provided to foster engagement, and simulate conversation and knowledge sharing.
You have to be authorized to post a comment. Please, Login or Signup.