Final ID: 12
High HDL Cholesterol Is Associated With Reduced Reperfusion Injury And Favorable Functional Outcome Following Thrombectomy For Ischemic Stroke
Abstract Body: Introduction: Animal research suggests that HDL cholesterol (HDL-C) ameliorates reperfusion injury, a phenomenon that worsens clinical outcome following recanalization therapy for ischemic stroke.
Hypothesis: We hypothesized that higher HDL-C levels have a guarding effect against cerebral reperfusion injury in human stroke survivors treated with thrombectomy.
Methods: We included patients with anterior circulation large vessel occlusion (acLVO) stroke who underwent thrombectomy from 01/2017 to 01/2023 at a tertiary stroke center in Germany into a prospective registry study with retrospective analysis. We assessed the association of HDL-C serum levels and imaging indices of post interventional reperfusion injury (any intracerebral or subarachnoid bleeding involving the ischemic brain region on CT or MRT), functional outcome quantified via modified Rankin scale (mRS) at 90 days and neurological outcome via National Institutes of Health Stroke Scale (NIHSS) score at discharge using multivariable lasso logistic and linear regression adjusted for demographic, clinical and imaging characteristics. We performed sensitivity analysis applying propensity score matching and shift analysis using ordered logistic regression.
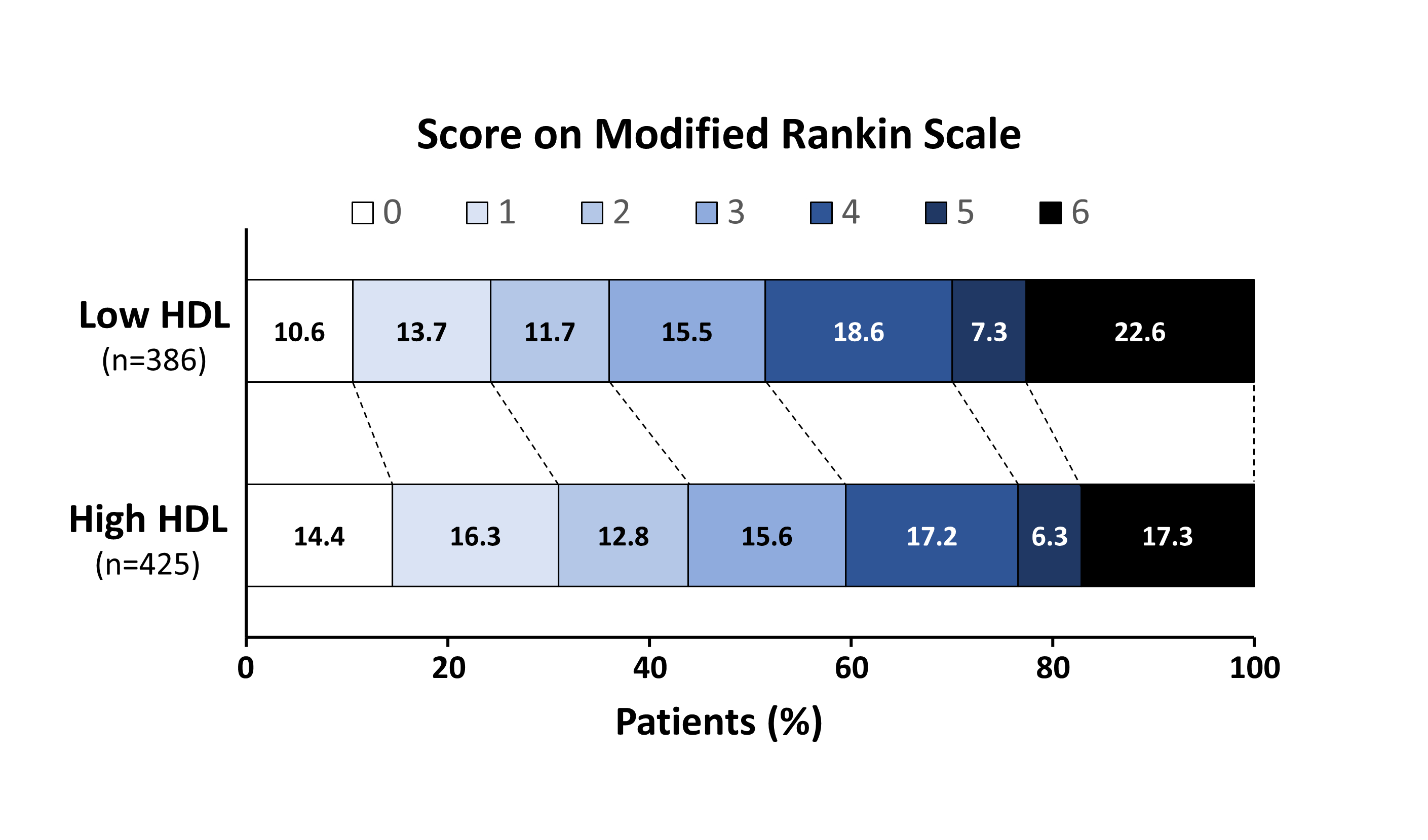
Results: In our study population of 811 acLVO patients treated with thrombectomy (420 females, median age 77 years [66-84, interquartile range]) reperfusion injury was associated with detrimental functional outcome (adjusted OR 2.87; 95% CI [1.86;4.41]; p=0.000). Higher HDL-C was associated with lower odds of reperfusion injury (adjusted OR 0.57; 95% CI [0.35;0.95]; p=0.03) and emerged as predictor of favorable functional outcome defined as 90-day mRS 0-2 (adjusted OR 0.57; 95% CI [0.34;0.99]; p=0.04) and alleviated neurological deficits with lower NIHSS score at discharge (ß=-2.51; 95CI% [-4.88; -1.30]; p=0.04). On propensity score analysis an HDL-C level exceeding the median (1.15 mmol/L) was associated with a 13.8 % decrease in the probability of reperfusion injury (ß=-0.14; 95CI% [-0.23; -0.05]; p=0.003). A significant shift of 90-day mRS distribution favoring high HDL is shown in the figure.
Conclusions: In patients undergoing thrombectomy for acLVO a higher level of HDL-C reduced the odds of reperfusion injury, which translated into improved functional and neurological outcome, hence constituting a possible target of adjunctive neuroprotective treatment.
Hypothesis: We hypothesized that higher HDL-C levels have a guarding effect against cerebral reperfusion injury in human stroke survivors treated with thrombectomy.
Methods: We included patients with anterior circulation large vessel occlusion (acLVO) stroke who underwent thrombectomy from 01/2017 to 01/2023 at a tertiary stroke center in Germany into a prospective registry study with retrospective analysis. We assessed the association of HDL-C serum levels and imaging indices of post interventional reperfusion injury (any intracerebral or subarachnoid bleeding involving the ischemic brain region on CT or MRT), functional outcome quantified via modified Rankin scale (mRS) at 90 days and neurological outcome via National Institutes of Health Stroke Scale (NIHSS) score at discharge using multivariable lasso logistic and linear regression adjusted for demographic, clinical and imaging characteristics. We performed sensitivity analysis applying propensity score matching and shift analysis using ordered logistic regression.
Results: In our study population of 811 acLVO patients treated with thrombectomy (420 females, median age 77 years [66-84, interquartile range]) reperfusion injury was associated with detrimental functional outcome (adjusted OR 2.87; 95% CI [1.86;4.41]; p=0.000). Higher HDL-C was associated with lower odds of reperfusion injury (adjusted OR 0.57; 95% CI [0.35;0.95]; p=0.03) and emerged as predictor of favorable functional outcome defined as 90-day mRS 0-2 (adjusted OR 0.57; 95% CI [0.34;0.99]; p=0.04) and alleviated neurological deficits with lower NIHSS score at discharge (ß=-2.51; 95CI% [-4.88; -1.30]; p=0.04). On propensity score analysis an HDL-C level exceeding the median (1.15 mmol/L) was associated with a 13.8 % decrease in the probability of reperfusion injury (ß=-0.14; 95CI% [-0.23; -0.05]; p=0.003). A significant shift of 90-day mRS distribution favoring high HDL is shown in the figure.
Conclusions: In patients undergoing thrombectomy for acLVO a higher level of HDL-C reduced the odds of reperfusion injury, which translated into improved functional and neurological outcome, hence constituting a possible target of adjunctive neuroprotective treatment.
More abstracts on this topic:
A novel method for measuring HDL-bound unconjugated bilirubin using an eel fluorescent protein reveals its association with reduced coronary artery disease
Fujioka Tomoo, Iino Takuya, Toh Ryuji, Harada Amane, Nagao Manabu, Shinohara Masakazu, Ishida Tatsuro, Otake Hiromasa
Association of Estimated Pulse Wave Velocity on Endovascular Treatment Outcome: A Secondary Analysis of the OPTIMAL-BP trialHan Minho, Joo Haram, Lee Hyungwoo, Heo Joonnyung, Jung Jae Wook, Kim Young Dae, Park Eunjeong, Nam Hyo Suk
Readers' Comments
We encourage you to enter the discussion by posting your comments and questions below.
Presenters will be notified of your post so that they can respond as appropriate.
This discussion platform is provided to foster engagement, and simulate conversation and knowledge sharing.
You have to be authorized to post a comment. Please, Login or Signup.
Rate this abstract
(Maximum characters: 500)