Final ID: WP256
Cognitive Outcomes in Acute Ischemic Stroke with Large Vessel Occlusion After Treatment with Endovascular Thrombectomy with and without Intravenous Thrombolysis
Abstract Body: Introduction: In acute stroke patients who receive revascularization with endovascular thrombectomy (EVT) alone vs intravenous thrombolysis (IVT) followed by EVT, combination treatment has shown improved outcomes measured by the modified Rankin Scale (mRS). However, neurocognitive outcomes beyond functional disability have not been sufficiently assessed.
Hypothesis: We hypothesize that neurocognitive outcomes will be improved with IVT + EVT compared to EVT alone.
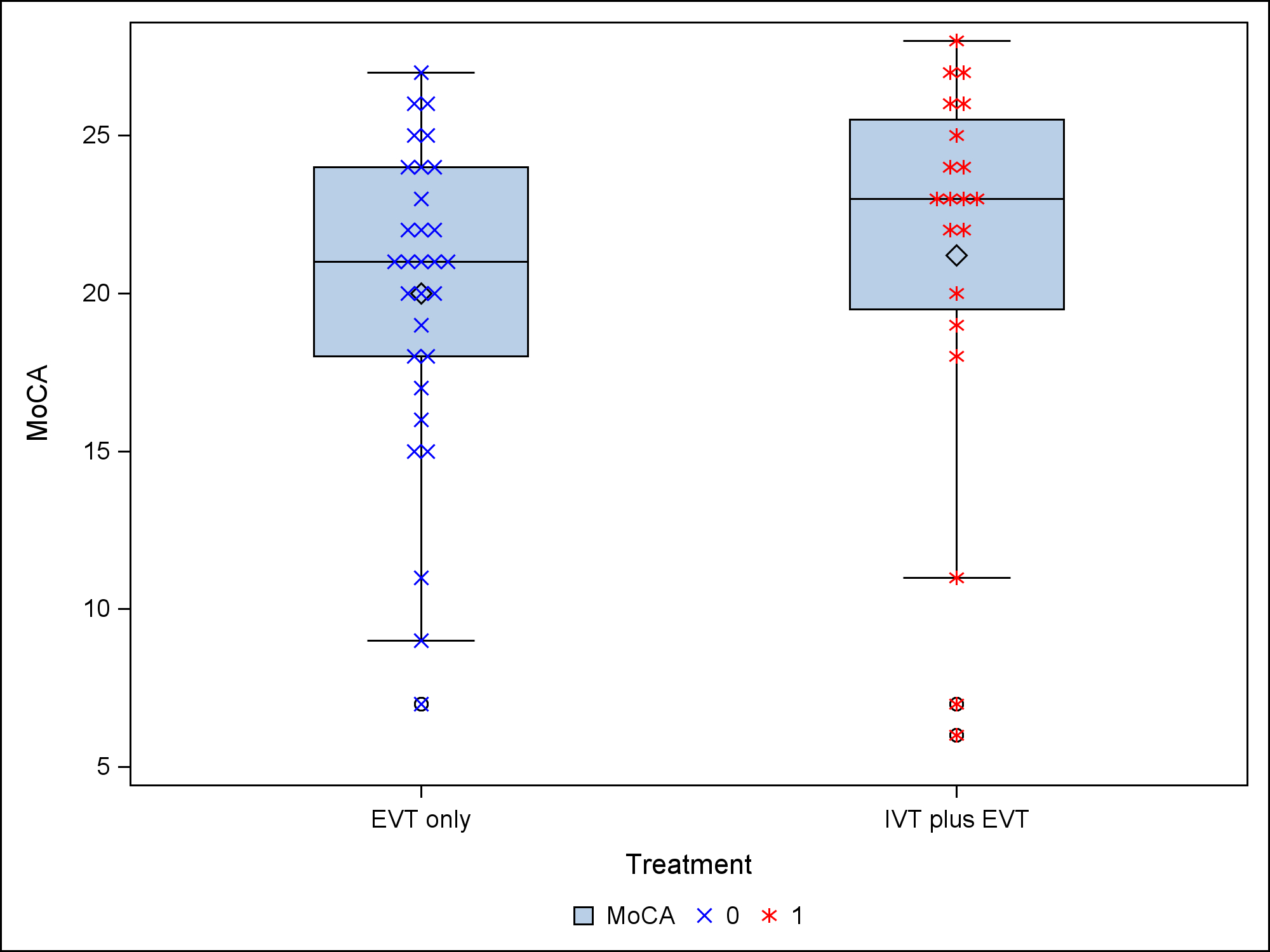
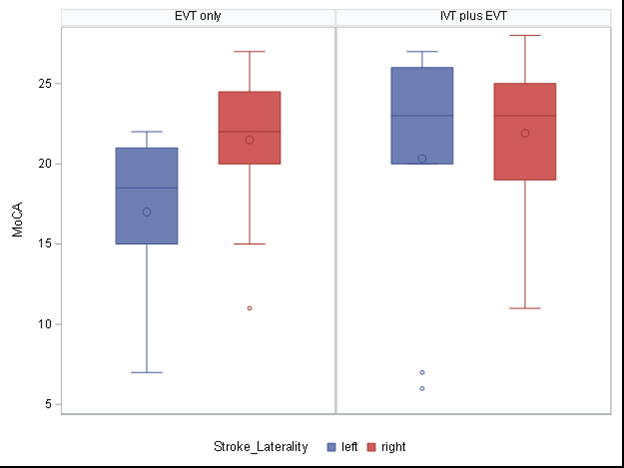
Methods: This prospective ongoing longitudinal study included patients with a first-ever ischemic stroke with large vessel occlusions admitted to our comprehensive stroke center who received EVT only vs IVT + EVT. Blinded investigators administered the Montreal Cognitive Assessment (MoCA) during the hospital stay. A linear model was used to estimate the difference in MoCA scores between the two treatment groups while adjusting for age, NIHSS obtained within 24 hours of MoCA, and pre-stroke mRS. A visual inspection of residuals was performed to check model assumptions. Box plots were utilized to compare MoCA differences across treatment groups, NIHSS scores, and stroke laterality.
Results: 50 participants had a mean age of 66.7 years (64% male). The mean post treatment NIHSS was 3.6, and the mean MoCA score was 20.5. The adjusted difference in MoCA scores between the treatment groups (IVT + EVT vs EVT only) was 0.83 points (95% CI –2.4 - 4.0), indicating no statistically significant difference. Higher NIHSS showed a trend toward negative association with MoCA scores, –0.41 (CI –0.90 - 0.07). For right sided strokes, there was minimal difference between treatment groups. However, for left sided strokes, there was a trend towards improved mean MoCA in the IVT + EVT group (20.3; CI 20.0 - 26.0) compared to EVT only (17.0; CI 15.0 - 21.0). The TICI revascularization score of 2c had the highest mean MoCA (22.1; CI 19.4 - 24.8), followed by TICI score of 3 (20.7; CI 18.9 - 22.7) and then 2b (16.6; CI 9.0 - 24.1).
Conclusion: There was no significant difference of MoCA with combination treatment vs EVT alone, but there was a trend showing improvement in combination treatment for left-sided strokes. There was also a trend showing decreased MoCA with higher NIHSS. We are currently assessing neurocognitive outcomes with a larger sample size post treatment and at 6 months post-stroke.
Hypothesis: We hypothesize that neurocognitive outcomes will be improved with IVT + EVT compared to EVT alone.
Methods: This prospective ongoing longitudinal study included patients with a first-ever ischemic stroke with large vessel occlusions admitted to our comprehensive stroke center who received EVT only vs IVT + EVT. Blinded investigators administered the Montreal Cognitive Assessment (MoCA) during the hospital stay. A linear model was used to estimate the difference in MoCA scores between the two treatment groups while adjusting for age, NIHSS obtained within 24 hours of MoCA, and pre-stroke mRS. A visual inspection of residuals was performed to check model assumptions. Box plots were utilized to compare MoCA differences across treatment groups, NIHSS scores, and stroke laterality.
Results: 50 participants had a mean age of 66.7 years (64% male). The mean post treatment NIHSS was 3.6, and the mean MoCA score was 20.5. The adjusted difference in MoCA scores between the treatment groups (IVT + EVT vs EVT only) was 0.83 points (95% CI –2.4 - 4.0), indicating no statistically significant difference. Higher NIHSS showed a trend toward negative association with MoCA scores, –0.41 (CI –0.90 - 0.07). For right sided strokes, there was minimal difference between treatment groups. However, for left sided strokes, there was a trend towards improved mean MoCA in the IVT + EVT group (20.3; CI 20.0 - 26.0) compared to EVT only (17.0; CI 15.0 - 21.0). The TICI revascularization score of 2c had the highest mean MoCA (22.1; CI 19.4 - 24.8), followed by TICI score of 3 (20.7; CI 18.9 - 22.7) and then 2b (16.6; CI 9.0 - 24.1).
Conclusion: There was no significant difference of MoCA with combination treatment vs EVT alone, but there was a trend showing improvement in combination treatment for left-sided strokes. There was also a trend showing decreased MoCA with higher NIHSS. We are currently assessing neurocognitive outcomes with a larger sample size post treatment and at 6 months post-stroke.
More abstracts on this topic:
A Multi-Tier, Natural-Language Processing Framework to Automate Labeling of Acute Cerebrovascular Events From Radiology Reports and Diagnosis Codes
Erekat Asala, Stein Laura, Delman Bradley, Karp Adam, Kupersmith Mark, Kummer Benjamin
Age at First Diagnosis of Atrial Fibrillation and Longitudinal Cognitive DeclineWang Yujie, Wang Bin, Cao Han, Tang Mingkun, Yao Chen, Zhang Ping, Li Dong
Readers' Comments
We encourage you to enter the discussion by posting your comments and questions below.
Presenters will be notified of your post so that they can respond as appropriate.
This discussion platform is provided to foster engagement, and simulate conversation and knowledge sharing.
You have to be authorized to post a comment. Please, Login or Signup.
Rate this abstract
(Maximum characters: 500)