Final ID: WP153
Identifying the Experiences and Longitudinal Needs of Stroke Survivors and Caregivers from Bedside to Community
Abstract Body: Introduction: Despite the high incidence rate of post-stroke anxiety and mood changes, there is limited evidence for the integration of emotional and mental health support resources into acute care and long-term recovery. In this international survey-based study, we seek to better understand the emotional and mental health needs of survivors and caregivers.
Methods: Participants were recruited via online advertising and advocacy groups. Eligibility included: ≥18 years, fluent in English, and identified as a brain injury survivor, caregiver, or healthcare worker. This analysis focuses on the stroke subgroup. Descriptive statistics were used for quantitative data and thematic analysis for qualitative responses.
Results: 410 individuals completed the survey (stroke: n=200). Most of them (n=158, 79%) were youth stroke survivors (aged <50 years). Both ischemic (n=59, 29%) and hemorrhagic stroke (n=141, 71%) survivors experienced an average of 3 impairments: fatigue was most common (n=150, 75%).
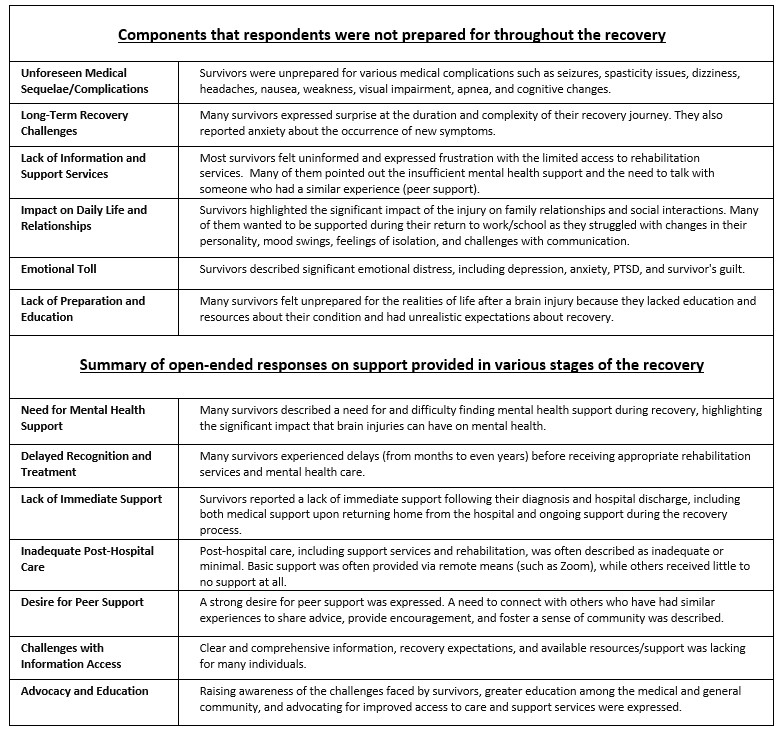
Surveyors reported a lack of overall emotional (n=152, 76%) and mental health support (n=139, 70%), insufficient communication about anticipated recovery (n=145, 73%), and a desire for more discussion on rehabilitation options (n=108, 54%). Table 1 presents a thematic analysis of recovery.
Most experienced a high level of anxiety ( ≥6.5/10) about long-term recovery (M =6.6, SD =2.6), emerging symptoms (M =6.7, SD =2.7), uncertainty about the future (M= 6.9, SD=2.7) and financial and return to work concerns (M=6.5, SD=3.1).
Many were unfamiliar with brain injury before their diagnosis (n=152, 76%) and reported that no information about emotional or mental support was shared at discharge (n=136, 68%). Searching the internet was utilized most for seeking information (n=144, 72%).
A majority had no contacts who had lived brain injury experience (n=150, 75%) but desired someone to talk to in their transition from bedside to community; with a preference for in-person peer support. Qualitative analyses outline the ideal supporter as empathetic, resourceful, knowledgeable about recovery, and honest.
Conclusion: The survey indicates a lack of and need for early integration of emotional and mental health support services and comprehensive informational resources into longitudinal recovery plans. This data could guide future peer support programs and inform other research studies by emphasizing the importance of continuous dialogue with community partners and people with lived experience.
Methods: Participants were recruited via online advertising and advocacy groups. Eligibility included: ≥18 years, fluent in English, and identified as a brain injury survivor, caregiver, or healthcare worker. This analysis focuses on the stroke subgroup. Descriptive statistics were used for quantitative data and thematic analysis for qualitative responses.
Results: 410 individuals completed the survey (stroke: n=200). Most of them (n=158, 79%) were youth stroke survivors (aged <50 years). Both ischemic (n=59, 29%) and hemorrhagic stroke (n=141, 71%) survivors experienced an average of 3 impairments: fatigue was most common (n=150, 75%).
Surveyors reported a lack of overall emotional (n=152, 76%) and mental health support (n=139, 70%), insufficient communication about anticipated recovery (n=145, 73%), and a desire for more discussion on rehabilitation options (n=108, 54%). Table 1 presents a thematic analysis of recovery.
Most experienced a high level of anxiety ( ≥6.5/10) about long-term recovery (M =6.6, SD =2.6), emerging symptoms (M =6.7, SD =2.7), uncertainty about the future (M= 6.9, SD=2.7) and financial and return to work concerns (M=6.5, SD=3.1).
Many were unfamiliar with brain injury before their diagnosis (n=152, 76%) and reported that no information about emotional or mental support was shared at discharge (n=136, 68%). Searching the internet was utilized most for seeking information (n=144, 72%).
A majority had no contacts who had lived brain injury experience (n=150, 75%) but desired someone to talk to in their transition from bedside to community; with a preference for in-person peer support. Qualitative analyses outline the ideal supporter as empathetic, resourceful, knowledgeable about recovery, and honest.
Conclusion: The survey indicates a lack of and need for early integration of emotional and mental health support services and comprehensive informational resources into longitudinal recovery plans. This data could guide future peer support programs and inform other research studies by emphasizing the importance of continuous dialogue with community partners and people with lived experience.
More abstracts on this topic:
A Case Series of Papillary Fibroelastomas on the Coumadin ridge
Aboukhatwa Omar, Akiki Elias, Kurmann Reto, Larson Kathryn, Keeney Michael, Bois Melanie, Klarich Kyle
Accessibility of Vascular Surgeons in Communities at High Risk for Peripheral Artery DiseaseQuinn Patrick, Armstrong Molly, Campbell Drayson, Corriere Matthew
Readers' Comments
We encourage you to enter the discussion by posting your comments and questions below.
Presenters will be notified of your post so that they can respond as appropriate.
This discussion platform is provided to foster engagement, and simulate conversation and knowledge sharing.
You have to be authorized to post a comment. Please, Login or Signup.
Rate this abstract
(Maximum characters: 500)