Final ID: TMP10
Impact of eicosapentaenoic acids and cilostazol in patients with intracranial arterial disease
METHODS: Patients with symptomatic and asymptomatic intracranial artery stenosis treated and followed at our institution from January 2009 to December 2023 were included in this study: 198 ICAD lesions in 155 patients (mean follow-up 11 months) were retrospectively evaluated. Each patient was divided into antiplatelet therapy alone (AA) (monotherapy (MT) or CT), antiplatelet therapy plus statin (AS), and antiplatelet therapy plus statin and EPA (AE). Antiplatelet drug monotherapy was aspirin, clopidogrel, or prasugrel and combination therapy was any of them plus cilostazol. ICAD was assessed by MRA and the stenosis rate was calculated by the warfarin-aspirin symptomatic intracranial disease (WASID) method.
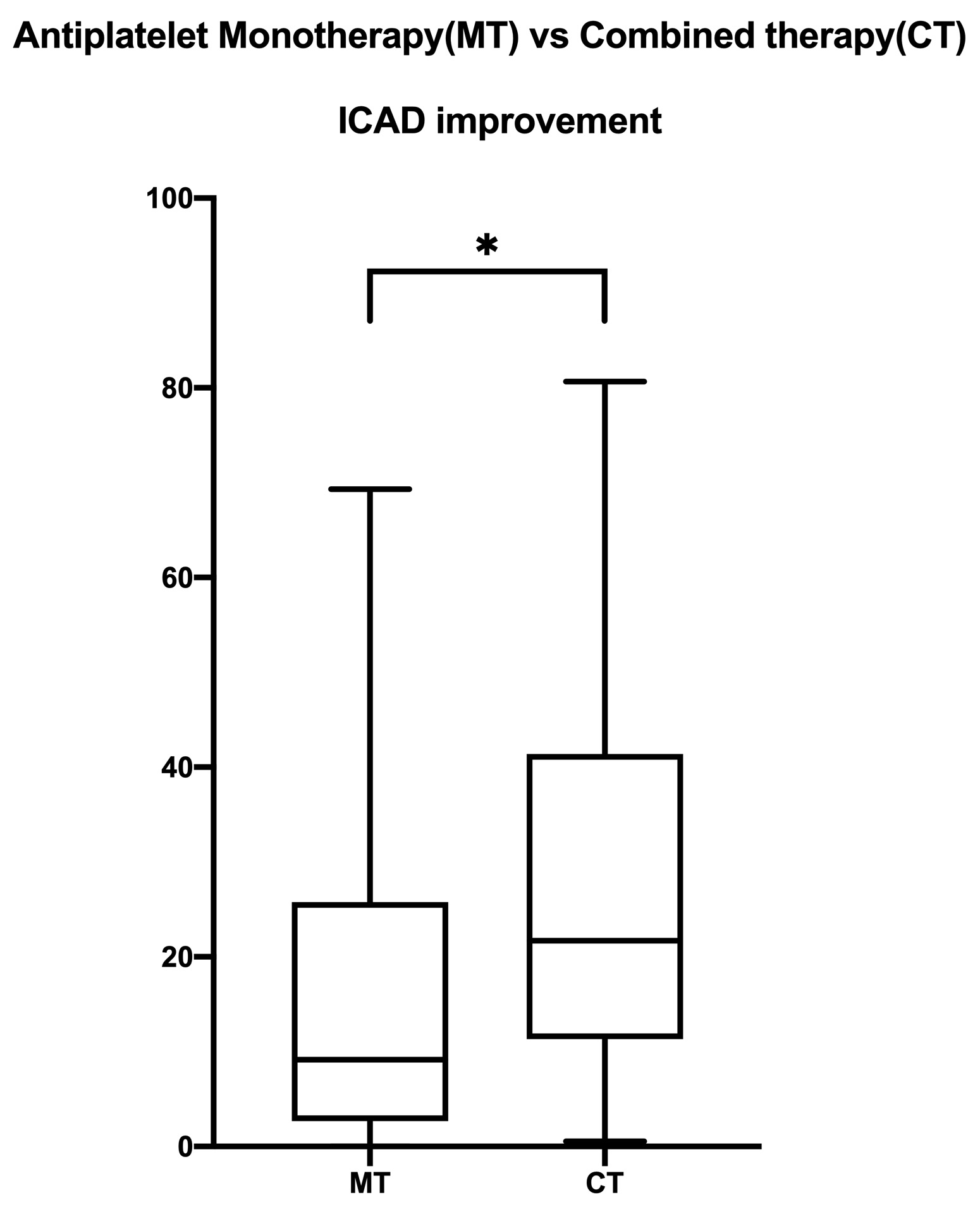
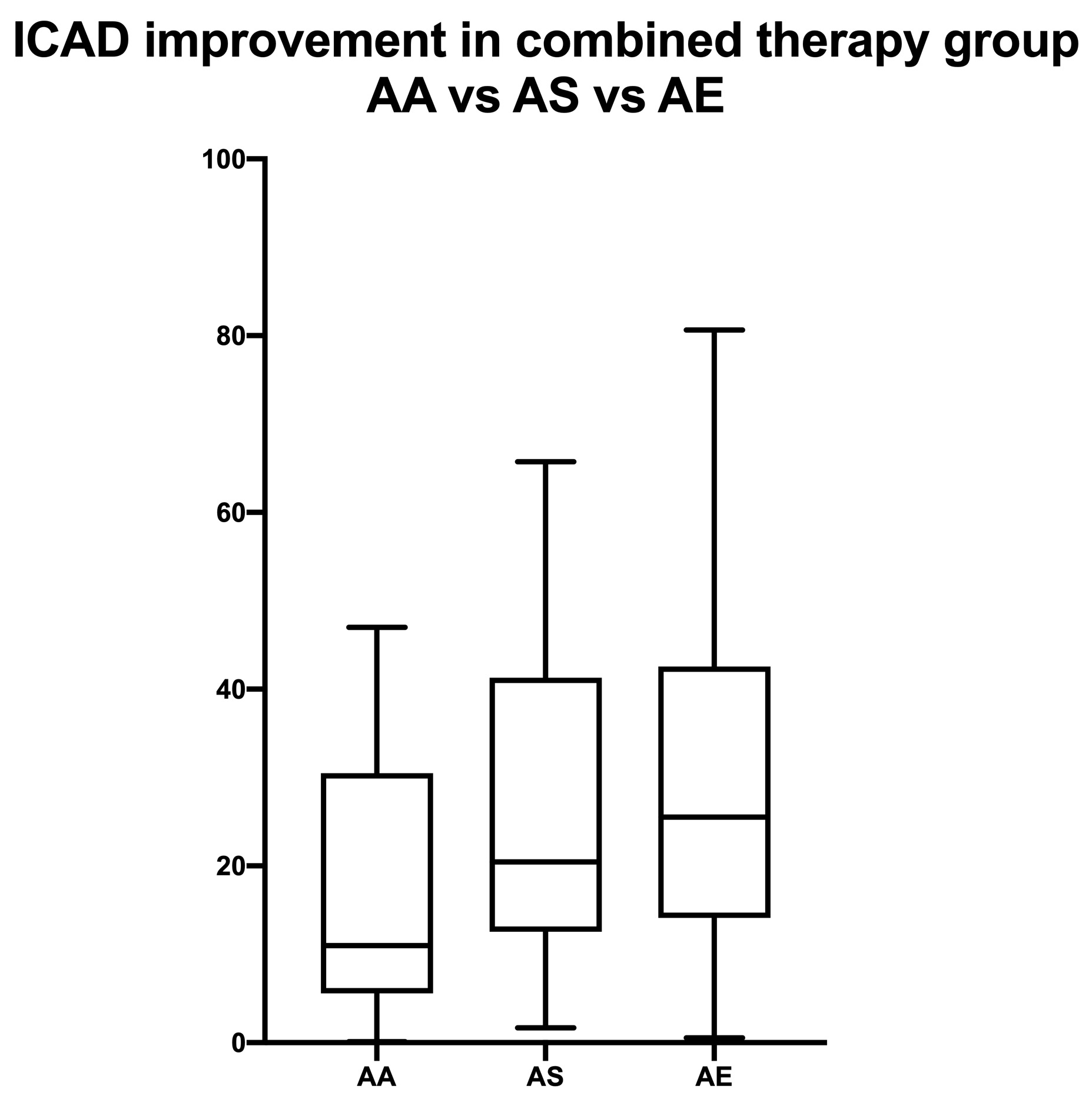
RESULTS: The improvement in stenosis was significantly better with CT than with MT (Median% interquartile range(IQR)= CT: 21.71% (11.33-41.40) vs. MT: 9.15% (2.69-25.78), P<0.0001 Mann-Whitney test). Within the CT group, the AE group showed the greatest improvement in stenosis (Median% (IQR)= AA: 10.95% (5.55-30.45) vs AS: 20.41% (12.54-41.26) vs AE: 25.51% (14.11-42.55), Kruskal-Wallis test p:0.0181), while there were no significant differences between the MT groups (Kruskal-Wallis test p:0.7185). Stroke recurrence rates were 16.2% in the AA group, 13.8% in the AS group, and 5.9% in the AE group, with no significant difference, but a trend toward lower recurrence rates in the AE group was observed; in a comparison of the CT+AE group with the MT+AA group, the CT+AE group had significantly lower recurrence rates than the MT+AA group (Fisher's exact test P: 0.0455).
CONCLUSION: Cilostazol and EPA added to the conventional therapy was associated with less stroke recurrence, and it also showed significant regression in ICAD. Larger studies should investigate the role of cilostazol and EPA in stroke recurrence and plaque regression.
More abstracts on this topic:
Tomasello Alejandro, Hassan Ameer, Miller Samantha, Zapata-arriaza Elena, De Alboniga-chindurza Asier, Bergui Mauro, Molinaro Stefano, Sousa Joao Andre, Gomes Fábio, Alexandre Andrea, Pedicelli Alessandro, Salcuni Andrea, Hofmeister Jeremy, Machi Paolo, Scarcia Luca, Kalsoum Erwah, Amorim José, Meira Torcato, Ortega-gutierrez Santiago, Rodriguez Aaron, Renieri Leonardo, Capasso Francesco, Kaesmacher Johannes, Gadea Marta, Romano Daniele, Barcena Eduardo, Abdalkader Mohamad, Perry Da Camara Catarina, Yavagal Dileep, Vega Pedro, Ozdemir Atilla Ozcan, Smajda Stanislas, Khalife Jane, Mujanovic Adnan, Biraschi Francesco, Castro Pedro, Siddiqui Adnan, Navia Pedro, Ntoulias Nikolaos, Velo Mariano, Zamarro Joaquin, Zaidat Osama, Sierra-gomez Alicia, Marto Joao Pedro, Geyik Serdar, Requena Manuel, Senadim Songul, Piano Mariangela, Moreu Manuel, Lopez-frias Alfonso
Evolocumab added to statin is superior to statin alone in reversing symptomatic intracranial atherosclerotic stenosisLiu Yiyang, Hu Xinzhi, Yuan Weizhuang, Li Shun, Zhang Yuelun, Li Mingli, Xu Yan, Xu Wei-hai
Readers' Comments
We encourage you to enter the discussion by posting your comments and questions below.
Presenters will be notified of your post so that they can respond as appropriate.
This discussion platform is provided to foster engagement, and simulate conversation and knowledge sharing.
You have to be authorized to post a comment. Please, Login or Signup.