Final ID: WP186
Small Vessel Disease is Associated With Primary Aldosteronism in Acute Ischemic Stroke
Methods: We screened consecutive patients with AIS who participated in our prospective study to investigate the prevalence of PA and followed up for PA evaluation from October 2020 to December 2022. Inclusion criteria were patients with AIS hospitalized and diagnosed with hypertension. Exclusion criteria were patients taking medications affecting renin, aldosterone, and catecholamines. The screening criteria for PA was defined as the aldosterone-to-renin ratio > 200. Final diagnosis of PA was judged by endocrinologist if one of the captopril challenge test, saline infusion test, and furosemide-upright test was positive following discharge. We evaluated total SVD score based on white matter hyperintensities (separately scored by periventricular hyperintensity [PVH] and deep and subcortical white matter hyperintensity), cerebral microbleeds (CMBs; categorized into deep, lobar, and infratentorial lesions), enlarged perivascular spaces (separately scored in basal ganglia and centrum semiovale), and old lacunes on MRI.
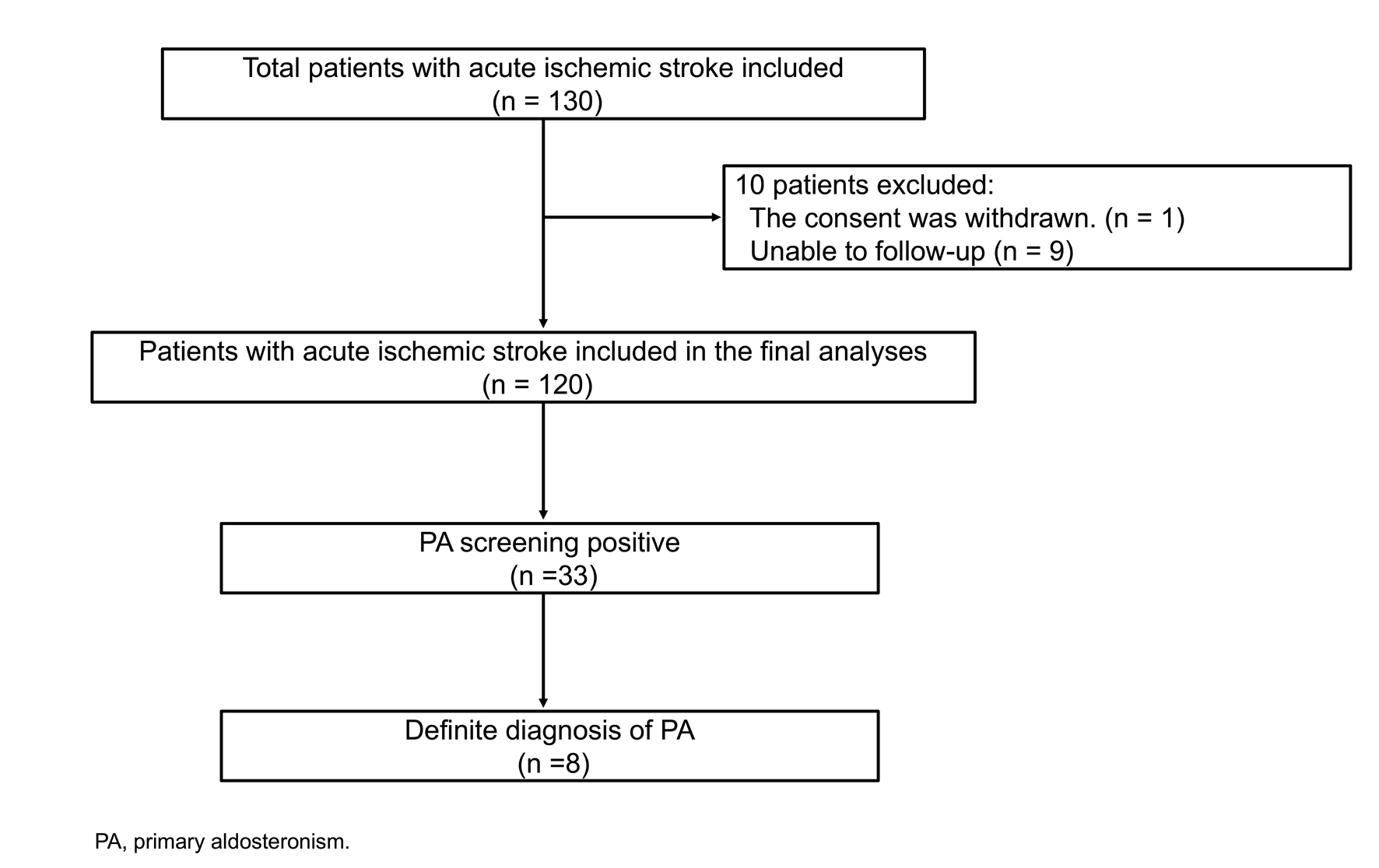
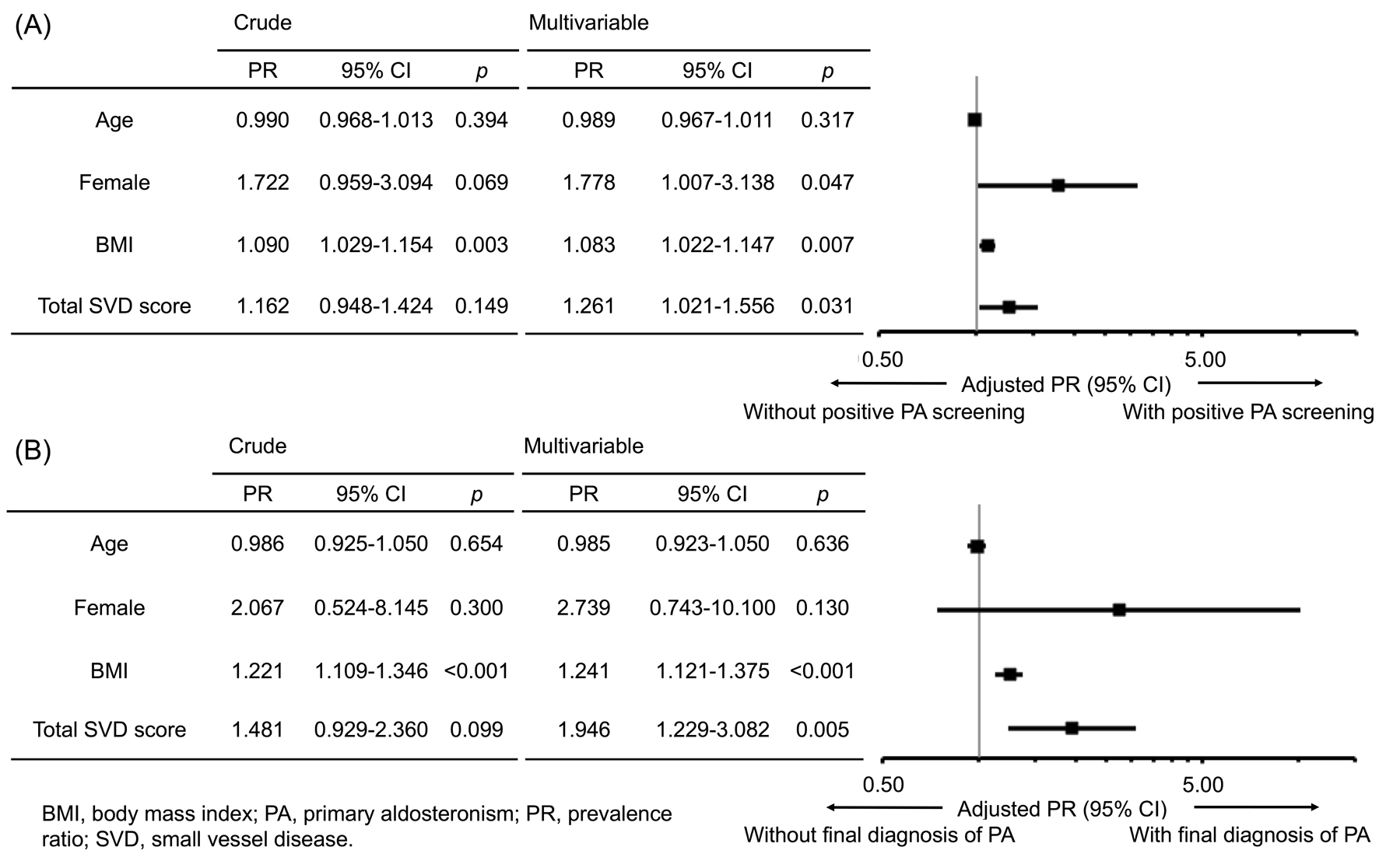
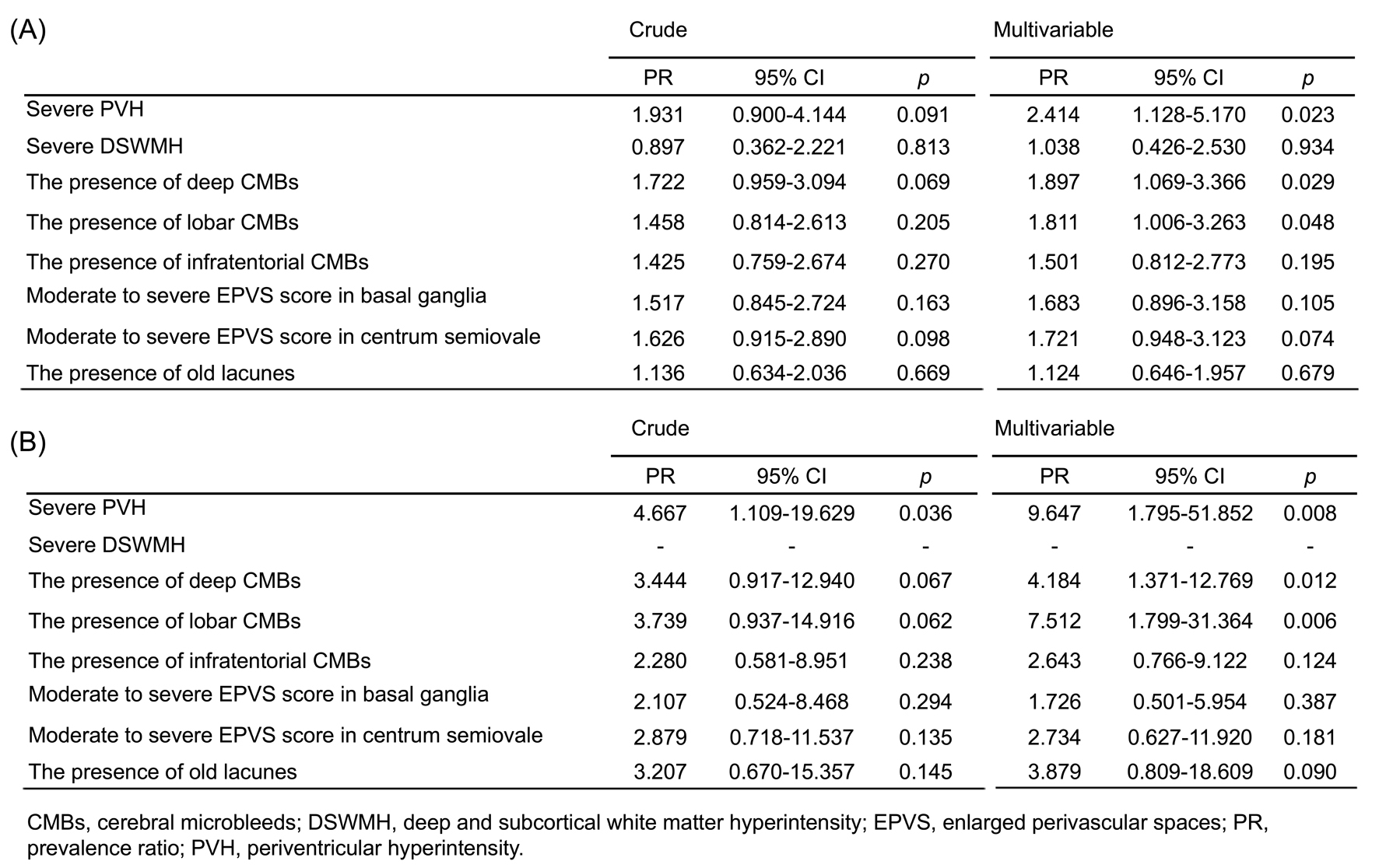
Results: We included 120 patients with AIS (93 [78%] male, median age 62 years, Figure 1). The screening for PA was positive in 33 (28%) patients and 8 (7%) patients were finally diagnosed with definite PA. In Poisson regression analysis with a robust variance estimator, total SVD score was related to positive PA screening (prevalence ratio [PR] 1.261, 95% CI 1.021-1.556, p = 0.031) and definite PA diagnosis (PR 1.946, 95% CI 1.229-3.082, p = 0.005, Figure 2). In terms of each SVD marker, severe PVH, and deep and lobar CMBs were associated with positive PA screening and definite PA diagnosis (Figure 3).
Conclusions: Twenty-eight percent of patients with AIS were positive for PA screening, and then about a quarter of them were confirmed as definite PA. SVD burden, especially PVH, and deep and lobar CMBs, might be associated with positive screening and definite diagnosis of PA.
More abstracts on this topic:
Chakravarthula Nitin Ramanujam, Milani Marcus, Tessmer Megan, Staugaitis Abbey, Akimoto Kai, Markowitz Jeremy, Kalra Rajat, Nijjar Prabhjot, Streib Christopher
Personal Care Product Usage Patterns And Hypertension In U.S. Women From The Sister StudyLim Jungeun, Chang Che-jung, White Alexandra, Lo Shelton, Wang Hantao, Goodney Gabriel, Roger Veronique, Sandler Dale, Wong Jason
Readers' Comments
We encourage you to enter the discussion by posting your comments and questions below.
Presenters will be notified of your post so that they can respond as appropriate.
This discussion platform is provided to foster engagement, and simulate conversation and knowledge sharing.
You have to be authorized to post a comment. Please, Login or Signup.