Final ID: WP3
Large Vessel Recanalization with Thrombolysis Prior to Thrombectomy: Incidence, Outcomes, and Associations With Collateral Status
Methods: This was a retrospective study at a comprehensive stroke center that centralizes patient transfers for EVT from a network of 15 hospitals. Adult patients with an internal carotid artery or middle cerebral artery LVO who received IVT and did not undergo EVT within one hour of LVO diagnosis were included. Clinical and radiographic information at the time of LVO diagnosis were collected. Collateral status was graded using the Tan score (Tan CS). LVR was defined as vessel recanalization identified on repeat vessel imaging leading to a decision to defer EVT. The primary endpoint was infarct progression defined as decrease in ASPECTS of two or more. The secondary endpoint was 90-day modified Rankin Scale (mRS) outcomes. Multivariable logistic regression models were used to adjust for various confounders.
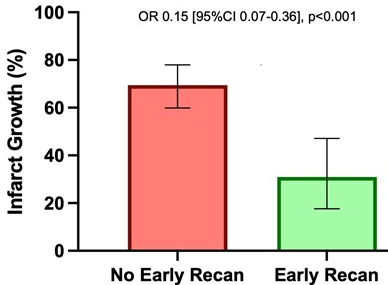
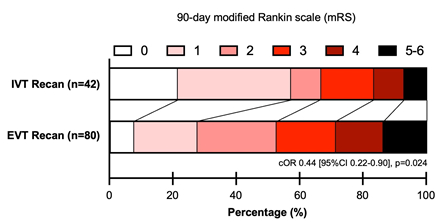
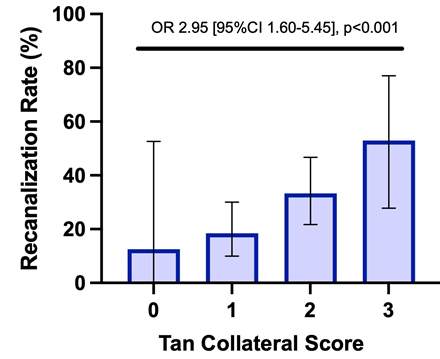
Results: Of the 150 patients included, 42 (28.0%) experienced LVR prior to EVT. LVR patients had lower NIH Stroke Scale (p=0.006) and higher Tan CS (p=0.019). In multivariable analyses, LVR was associated with significantly lower odds of infarct growth (OR 0.15 [95%CI 0.07-0.36], p<0.001), and compared with patients who underwent successful EVT recanalization, lower 90-day mRS (common OR 0.44 [95%CI 0.22-0.90], p=0.024). Higher Tan CS was significantly associated with higher odds of LVR (2.95 [95%CI 1.60-5.45], p<0.001), and both collateral status and LVR were independently associated with lower odds of infarct growth (0.34 [95%CI 0.18-0.63], p<0.001 and OR 0.21 [95%CI 0.09-0.52], p<0.001, respectively).
Conclusions: LVR with IVT prior to EVT was significantly associated with lower odds of infarct progression and better clinical outcomes. Better collateral circulation was independently associated with both higher odds of LVR, as well as lower odds of infarct progression. In conclusion, these findings suggest the clinical benefit of LVR for patients who cannot receive timely EVT and highlight the potential for modulating collaterals with the goal of limiting infarct growth and maximizing the odds of LVR.
More abstracts on this topic:
Shoemaker Camella, Shugrue Leah, Coccia Michael, Bakradze Ekaterina, Shapshak Dag, Gropen Toby, Thompson Karen, Taylor Danielle, Morrison Amanda, Stallings Ashley, Shipley Sarah, Jones Tamicka, Rafferty Rachael, Reid Tonya
A distinct clot transcriptomic signature is associated with atrial fibrillation-derived ischemic stroke in the INSIGHT RegistrySeah Carina, Rivet Dennis, Fraser Justin, Kellner Christopher, Devarajan Alex, Vicari James, Dabney Alan, Baltan Selva, Sohrabji Farida, Pennypacker Keith, Nanda Ashish, Woodward Britton
Readers' Comments
We encourage you to enter the discussion by posting your comments and questions below.
Presenters will be notified of your post so that they can respond as appropriate.
This discussion platform is provided to foster engagement, and simulate conversation and knowledge sharing.
You have to be authorized to post a comment. Please, Login or Signup.