Final ID: 2
Endovascular thrombectomy plus intravenous thrombolysis versus endovascular thrombectomy alone in patients with large core infarct
Abstract Body: Background: For patients meeting eligibility criteria, endovascular thrombectomy (EVT) remains the gold standard treatment for acute ischemic stroke (AIS) caused by large vessel occlusion (LVO). A few randomized trials have investigated EVT in AIS-LVO with large ischemic infarcts (LII). We studied the impact of intravenous thrombolysis (IVT) on the outcomes of EVT in those patients.
Methods: We conducted a meta-analysis using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) checklist and the Cochrane Handbook of Systematic Reviews and Interventions. We searched 4 databases (PubMed, Scopus, Web of Science, and Cochrane CENTRAL) from inception till June 11, 2024. We performed our analysis with RevMan utilizing a pooled risk ratio (RR) with a 95% confidence interval (CI).
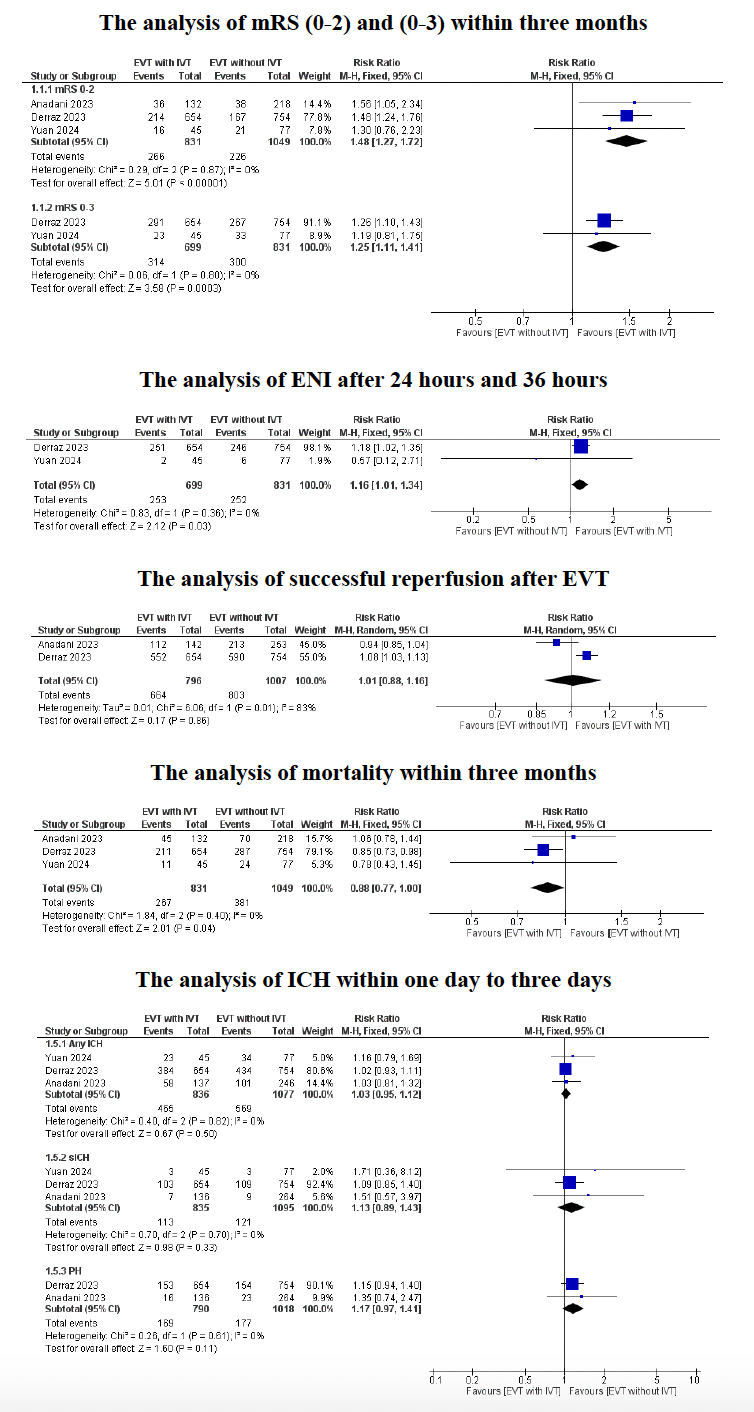
Results: Three studies with a total of 1,927 patients investigated EVT with and without IVT in AIS-LVO patients with LII. All 3 studies reported on modified Rankin Scale (mRS) score of 0-2 at 3 months, (831 patients in the EVT+IVT group and 1,049 patients in the EVT-only group), with a statistically significant difference favoring EVT+IVT (RR: 1.48, 95%CI: 1.27, 1.72, P< 0.00001). Two studies reported on mRS score of 0-3 (699 patients in the EVT+IVT group and 831 patients in the EVT-only group). The analysis also favored EVT+IVT (RR: 1.25, 95%CI: 1.11, 1.41, P= 0.0003). Two studies reported on early neurological improvement (ENI) after 24 and 36 hours (699 patients in the EVT+IVT group and 831 patients in the EVT-only group). The analysis revealed a statistically significant difference favoring EVT+IVT (RR: 1.16, 95%CI: 1.01, 1.34, P= 0.03). Two studies reported on successful reperfusion after EVT with no statistically significant difference between the two groups (RR: 1.01, 95%CI: 0.88, 1.16, P= 0.86). All 3 studies reported on mortality (831 patients in the EVT+IVT group and 1,049 patients in the EVT-only group), and the analysis favored EVT+IVT (RR: 0.88, 95%CI: 0.77, 1, P= 0.04). Lastly, our subgroup analysis did not favor any of the two groups across different types of intracranial hemorrhage (ICH).
Conclusion: Our results indicate a beneficial impact of IVT on the clinical outcomes of EVT in AIS-LVO patients with LII regarding functional outcomes and early neurological improvement. IVT was also associated with a lower mortality rate but not with an increased risk of ICH. More studies of larger sample sizes are needed to corroborate such results.
Methods: We conducted a meta-analysis using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) checklist and the Cochrane Handbook of Systematic Reviews and Interventions. We searched 4 databases (PubMed, Scopus, Web of Science, and Cochrane CENTRAL) from inception till June 11, 2024. We performed our analysis with RevMan utilizing a pooled risk ratio (RR) with a 95% confidence interval (CI).
Results: Three studies with a total of 1,927 patients investigated EVT with and without IVT in AIS-LVO patients with LII. All 3 studies reported on modified Rankin Scale (mRS) score of 0-2 at 3 months, (831 patients in the EVT+IVT group and 1,049 patients in the EVT-only group), with a statistically significant difference favoring EVT+IVT (RR: 1.48, 95%CI: 1.27, 1.72, P< 0.00001). Two studies reported on mRS score of 0-3 (699 patients in the EVT+IVT group and 831 patients in the EVT-only group). The analysis also favored EVT+IVT (RR: 1.25, 95%CI: 1.11, 1.41, P= 0.0003). Two studies reported on early neurological improvement (ENI) after 24 and 36 hours (699 patients in the EVT+IVT group and 831 patients in the EVT-only group). The analysis revealed a statistically significant difference favoring EVT+IVT (RR: 1.16, 95%CI: 1.01, 1.34, P= 0.03). Two studies reported on successful reperfusion after EVT with no statistically significant difference between the two groups (RR: 1.01, 95%CI: 0.88, 1.16, P= 0.86). All 3 studies reported on mortality (831 patients in the EVT+IVT group and 1,049 patients in the EVT-only group), and the analysis favored EVT+IVT (RR: 0.88, 95%CI: 0.77, 1, P= 0.04). Lastly, our subgroup analysis did not favor any of the two groups across different types of intracranial hemorrhage (ICH).
Conclusion: Our results indicate a beneficial impact of IVT on the clinical outcomes of EVT in AIS-LVO patients with LII regarding functional outcomes and early neurological improvement. IVT was also associated with a lower mortality rate but not with an increased risk of ICH. More studies of larger sample sizes are needed to corroborate such results.
More abstracts on this topic:
Association of Automated Anatomical Vascular Measurements and Procedural Outcomes in Patients undergoing Endovascular Treatment of Stroke
Sastre Blanca, Canals Pere, Garcia-tornel Garcia-camba Alvaro, Ribo Marc
A multifaceted family intervention for blood pressure management in rural China: an open label, parallel group, cluster randomized trial (Healthy Family Program)Jiang Chao, Dong Jianzeng, Cai Jun, Anderson Craig, Du Xin, Tang Yangyang, Han Rong, Song Yanna, Wang Chi, Lin Xiaolei, Yi Yang, Rodgers Anthony, Ma Changsheng
Readers' Comments
We encourage you to enter the discussion by posting your comments and questions below.
Presenters will be notified of your post so that they can respond as appropriate.
This discussion platform is provided to foster engagement, and simulate conversation and knowledge sharing.
You have to be authorized to post a comment. Please, Login or Signup.
Rate this abstract
(Maximum characters: 500)