Final ID: TMP58
Impact of DWI-ADC Mismatch on Infarct Progression and Endovascular Thrombectomy Outcomes in Acute Stroke
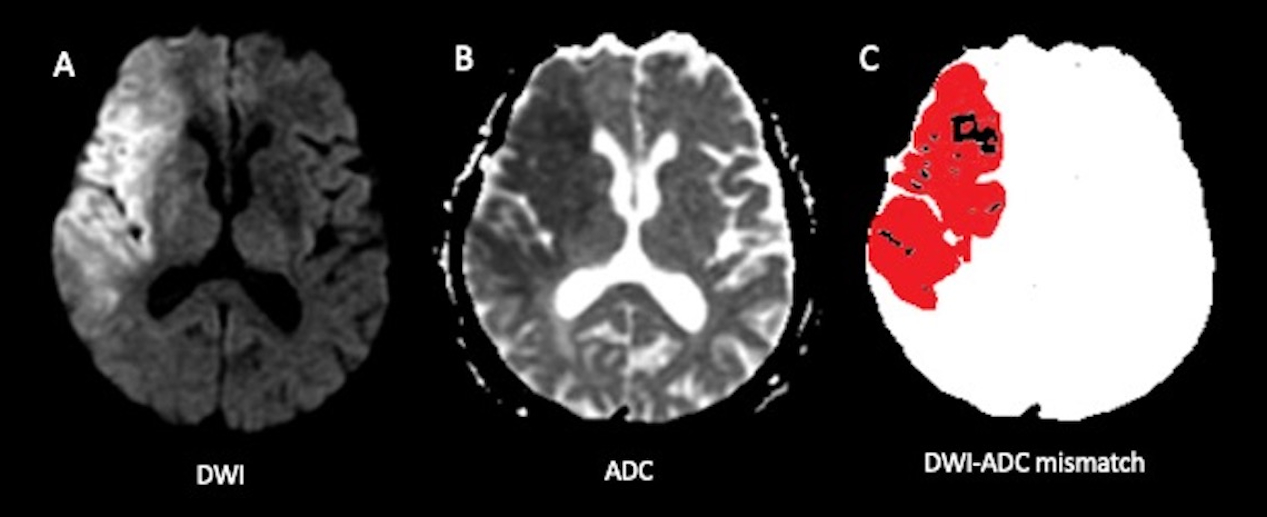
Introduction: An apparent diffusion coefficient (ADC) threshold of ≤ 620 × 10-6 mm2/s identifies irreversible infarcts and guides endovascular thrombectomy (EVT) decisions. However, in hyperacute ischemic infarcts, diffusion-weighted imaging (DWI) hyperintense lesions can show varying ADC values. This study investigates DWI-ADC mismatch, defined as the significant difference between DWI hyperintense lesion volume and ADC ≤ 620 × 10-6 mm2/s volume.
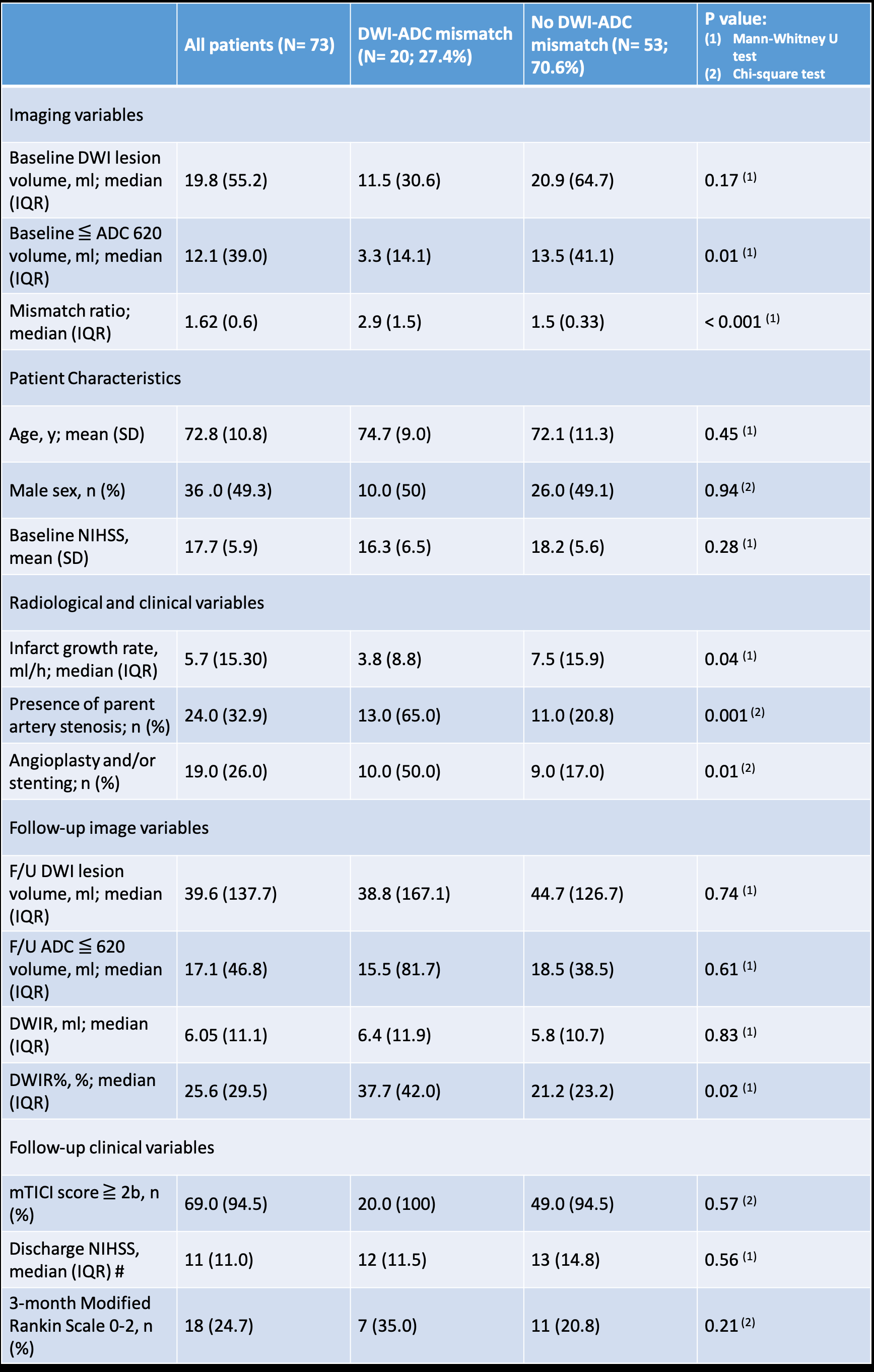
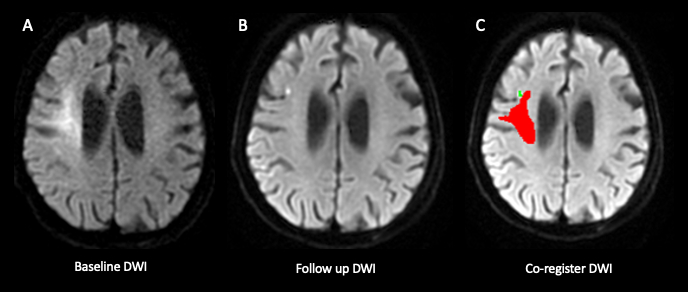
Methods: This retrospective, single-center study included patients with acute large vessel occlusion in the anterior circulation who: (1) underwent MRI within 24 hours of stroke onset, (2) received EVT, and (3) had follow-up MRI within 5 days of EVT from January 2018 to January 2020. Neuroradiologists segmented DWI hyperintense infarcts with ADC hypointensity on pre- and post-EVT MRI, using Fluid-attenuated inversion recovery (FLAIR) sequences to avoid T2 shine-through effects. The DWI/ADC volume ratio was calculated by dividing DWI volume by ADC ≤ 620 × 10-6 mm2/s volume. DWI-ADC mismatch was defined as a DWI/ADC ratio ≥ 2, with no mismatch indicated by a ratio < 2. Final infarct segmentation included hemorrhagic transformation. DWI lesion reversal (DWIR) was defined as the volume of normal-appearing voxels on follow-up DWI but previously hyperintense. DWIR% = (DWIR/baseline DWI volume) × 100 was calculated. We compared demographics, radiological findings, clinical outcomes, and follow-up results between mismatch and no mismatch groups.
Results: Among 73 patients, 20 (27.4%) had DWI-ADC mismatch. Baseline demographics and National Institutes of Health Stroke Scale (NIHSS) were similar between groups. The DWI/ADC ratio was higher in the mismatch group (2.9 vs. 1.5, P < 0.0001). Follow-up lesion volumes and functional outcomes were similar; however, the mismatch group showed a slower infarct growth rate (3.8 ml/h vs. 7.5 ml/h, P = 0.04), a higher likelihood of parent artery stenosis (65% vs. 20.8%, P < 0.001), and increased need for angioplasty or stenting (50% vs. 17%, P < 0.001). The mismatch group also had a higher DWIR% (37.7% vs. 21.2%, P = 0.02).
Conclusions: DWI-ADC mismatch is associated with slower infarct growth, greater likelihood of parent artery stenosis, increased need for angioplasty or stenting, and more DWI lesion reversal in anterior circulation large vessel occlusion patients undergoing EVT. These findings suggest DWI-ADC mismatch could be important in EVT decision-making and outcome prediction.
More abstracts on this topic:
He Lihao, Young Martin E, Rowe Glenn, Prabhu Sumanth, Sethu Palaniappan, Xie Min, Chen Yunxi, Chu Yuxin, Hua Yutao, Cai Junyan, He Jin, Benavides Gloria, Darley-usmar Victor, Ballinger Scott
Attenuating Post-stroke Ischemia Reperfusion Injury: Establishing the Efficacy of Disodium Malonate in a Clinically Relevant Sheep ModelSorby-adams Annabel, Murphy Mike, Sharkey Jessica, Prag Hiran, Turner Renee, Skein Keziah, Guglietti Bianca, Pullan Caitlin, Williams Georgia, Krieg Thomas
Readers' Comments
We encourage you to enter the discussion by posting your comments and questions below.
Presenters will be notified of your post so that they can respond as appropriate.
This discussion platform is provided to foster engagement, and simulate conversation and knowledge sharing.
You have to be authorized to post a comment. Please, Login or Signup.