Final ID: WMP120
Circulating Mucosal-Associated Invariant T Cells Are Associated with Acute Human Ischemic Stroke and Predict Poor Outcome
Abstract Body: Introduction: We previously demonstrated that Mucosal-associated Invariant T (MAIT) cells were involved in acute ischemic stroke by regulating neuroinflammation (JAHA 2021). This study aimed to clarify the dynamics and role of circulating peripheral MAIT cells in acute ischemic stroke patients.
Methods: We enrolled patients with acute ischemic stroke who admitted to Jichi Medical University Hospital, classifying them into severe (NIHSS ≥10) and mild (NIHSS <10) groups and outpatients were also enrolled as control. The proportion of circulating MAIT cells, activity (CD69+), and cytokine production (IFN-γ+ or IL-17+) were measured by flow cytometry on days 3, 10, and 17 post-stroke. Other innate-like T cells (iNKT and γδT cells) and CD4+ and CD8+ T cells were also analyzed for comparison. Associations between MAIT cell dynamics, function, and clinical outcomes were investigated.
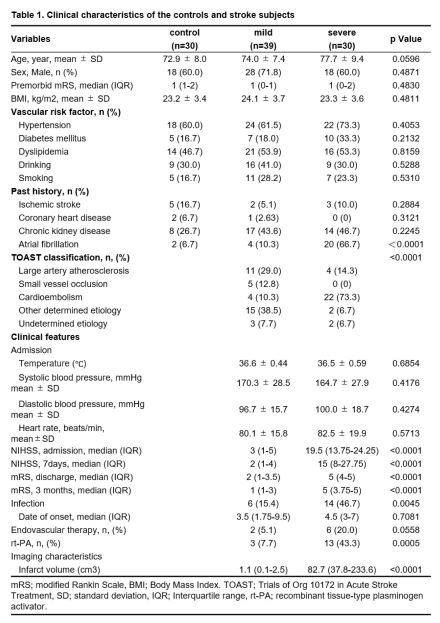
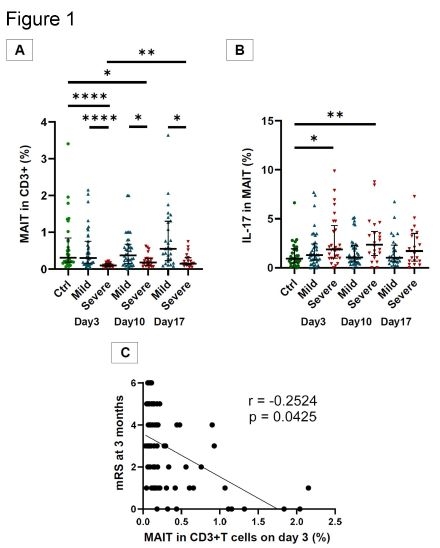
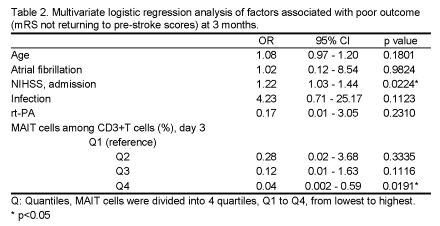
Results: A total of 30 severe stroke, 39 mild stroke, and 30 control subjects were included (Table 1). The mean ages were 77.7, 74.0, and 72.9 years, respectively. On day 3, the proportion of MAIT cells was significantly lower in the severe group, but not in the mild group, compared to control [severe, mild, and control (median): 0.10% (0.07-0.15), 0.31% (0.15-0.79), 0.31% (0.19-0.80); p <0.0001] (Figure 1A). In the severe group, the MAIT cell proportions gradually recovered by day 17. Severe stroke MAIT cells showed significantly higher CD69 positivity and IL-17 production rates from day 3 compared with the control (Figure 1B). The iNKT and γδT cell proportions showed no significant differences in both groups compared to the control. The MAIT cell proportion on day 3 was inversely correlated with the mRS at 3 months (r = -0.2524, p = 0.0425) (Figure 1C). Finally, stroke patients were categorized into four groups (Q1-Q4) based on their MAIT cell population quartile on day 3 and compared with their 3-month mRS. Multivariate analysis revealed that the Q4 group had a significantly lower probability of poor outcomes (defined as not returning to the pre-stroke mRS score at 3 months) than the Q1 group (OR 0.04, 95% CI 0.002-0.59, p = 0.0191) (Table 2).
Conclusions: We found dynamic changes in peripheral MAIT cells in acute human ischemic stroke. An early decrease in MAIT cells and an increase in activity and cytokine production might correlate with poor outcomes. MAIT cells could play a significant role in acute cerebral infarction and are associated with unfavorable outcomes.
Methods: We enrolled patients with acute ischemic stroke who admitted to Jichi Medical University Hospital, classifying them into severe (NIHSS ≥10) and mild (NIHSS <10) groups and outpatients were also enrolled as control. The proportion of circulating MAIT cells, activity (CD69+), and cytokine production (IFN-γ+ or IL-17+) were measured by flow cytometry on days 3, 10, and 17 post-stroke. Other innate-like T cells (iNKT and γδT cells) and CD4+ and CD8+ T cells were also analyzed for comparison. Associations between MAIT cell dynamics, function, and clinical outcomes were investigated.
Results: A total of 30 severe stroke, 39 mild stroke, and 30 control subjects were included (Table 1). The mean ages were 77.7, 74.0, and 72.9 years, respectively. On day 3, the proportion of MAIT cells was significantly lower in the severe group, but not in the mild group, compared to control [severe, mild, and control (median): 0.10% (0.07-0.15), 0.31% (0.15-0.79), 0.31% (0.19-0.80); p <0.0001] (Figure 1A). In the severe group, the MAIT cell proportions gradually recovered by day 17. Severe stroke MAIT cells showed significantly higher CD69 positivity and IL-17 production rates from day 3 compared with the control (Figure 1B). The iNKT and γδT cell proportions showed no significant differences in both groups compared to the control. The MAIT cell proportion on day 3 was inversely correlated with the mRS at 3 months (r = -0.2524, p = 0.0425) (Figure 1C). Finally, stroke patients were categorized into four groups (Q1-Q4) based on their MAIT cell population quartile on day 3 and compared with their 3-month mRS. Multivariate analysis revealed that the Q4 group had a significantly lower probability of poor outcomes (defined as not returning to the pre-stroke mRS score at 3 months) than the Q1 group (OR 0.04, 95% CI 0.002-0.59, p = 0.0191) (Table 2).
Conclusions: We found dynamic changes in peripheral MAIT cells in acute human ischemic stroke. An early decrease in MAIT cells and an increase in activity and cytokine production might correlate with poor outcomes. MAIT cells could play a significant role in acute cerebral infarction and are associated with unfavorable outcomes.
More abstracts on this topic:
A Multi-centre, Randomized, Controlled Study of External CounterPulsation for Patients with Recent Atherosclerotic Stroke (SPA)
Xiong Li, Chen Xiangyan, Leung Howan, Zhu Lixia, Leung Thomas, Wong Lawrence
Association between Increment of Near-Infrared Spectroscopy-Derived Cerebral Perfusion Index and Return of Spontaneous Circulation in Out-of-Hospital Cardiac Arrest Patients: A Prospective Observational StudyNishioka Norihiro, Kiguchi Takeyuki, Makino Yuto, Ninomiya Kouhei, Kamo Wataru, Kamada Tsuyoshi, Maeda Hideki, Iwami Taku
Readers' Comments
We encourage you to enter the discussion by posting your comments and questions below.
Presenters will be notified of your post so that they can respond as appropriate.
This discussion platform is provided to foster engagement, and simulate conversation and knowledge sharing.
You have to be authorized to post a comment. Please, Login or Signup.
Rate this abstract
(Maximum characters: 500)