Final ID: TP100
Predictors of Skilled Nursing Facility Length of Stay and Discharge after Aneurysmal Subarachnoid Hemorrhage
Methods: We conducted a retrospective review of a prospectively maintained database of aSAH patients treated at a single center from June 2016 to March 2024. Included patients were discharged from the hospital to an extended care facility. Patients were grouped by whether they were discharged from extended care to home and the estimated facility length of stay (LOS) was determined. Demographics, aSAH characteristics, hospital complications, and post-aSAH neurological status were analyzed. Predictors of extended care facility discharge to home were determined using independent-sample t-tests, Fisher analyses, and multivariable logistic regression. Facility LOS predictors were identified using cumulative link modeling.
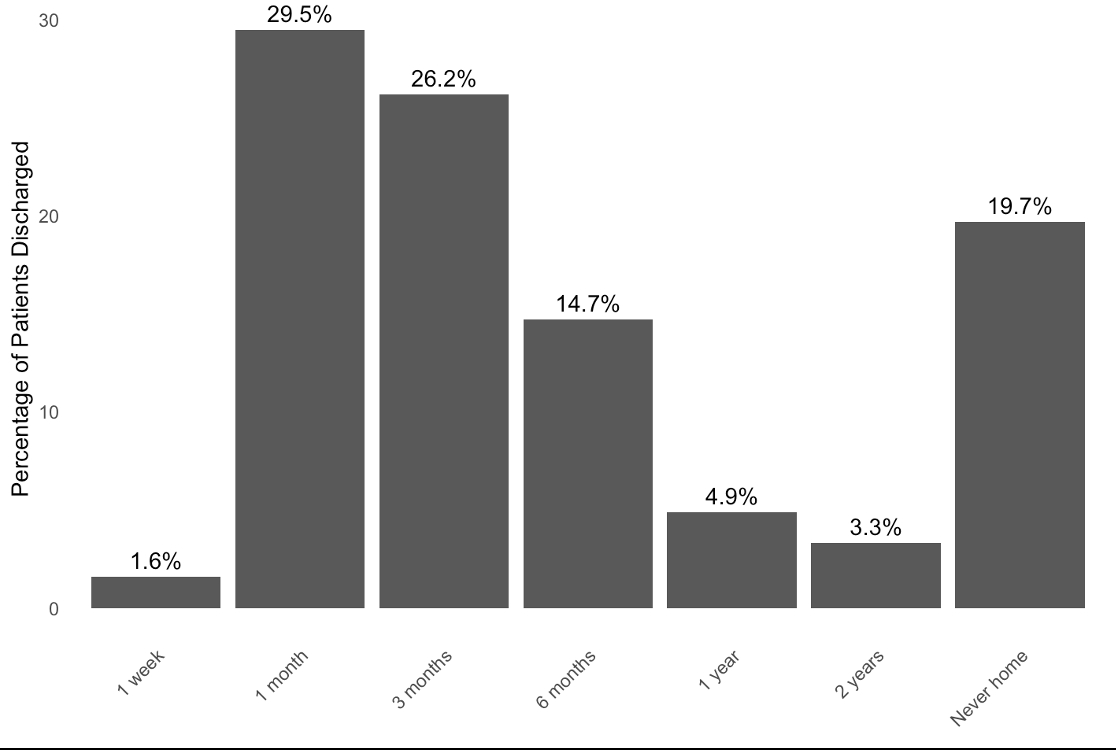
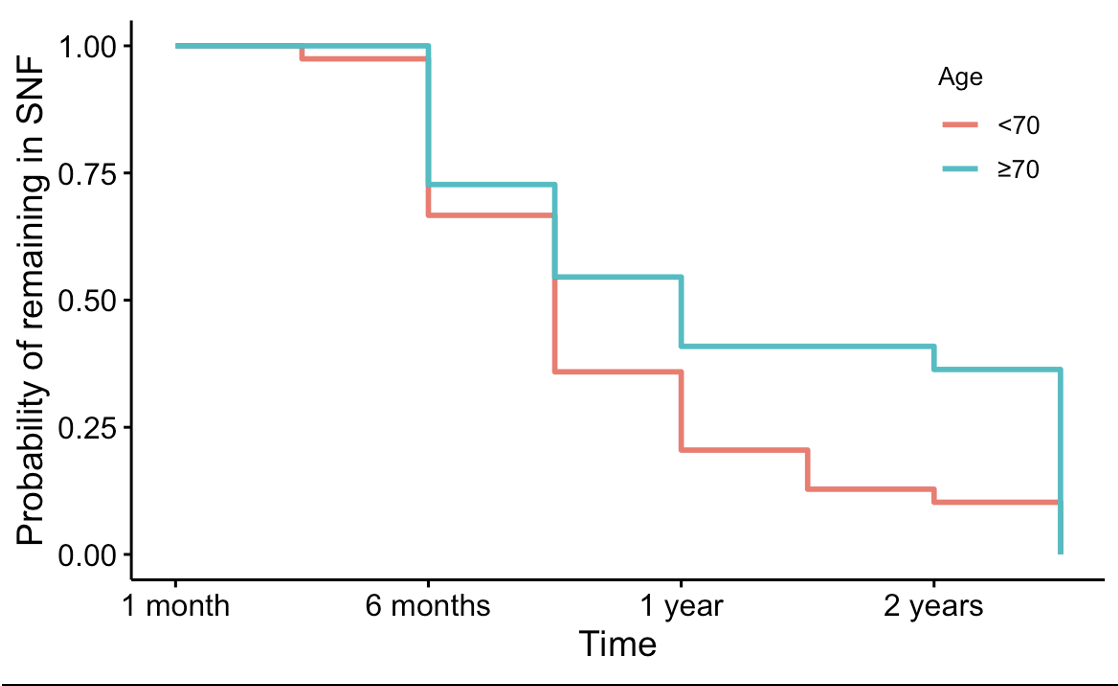
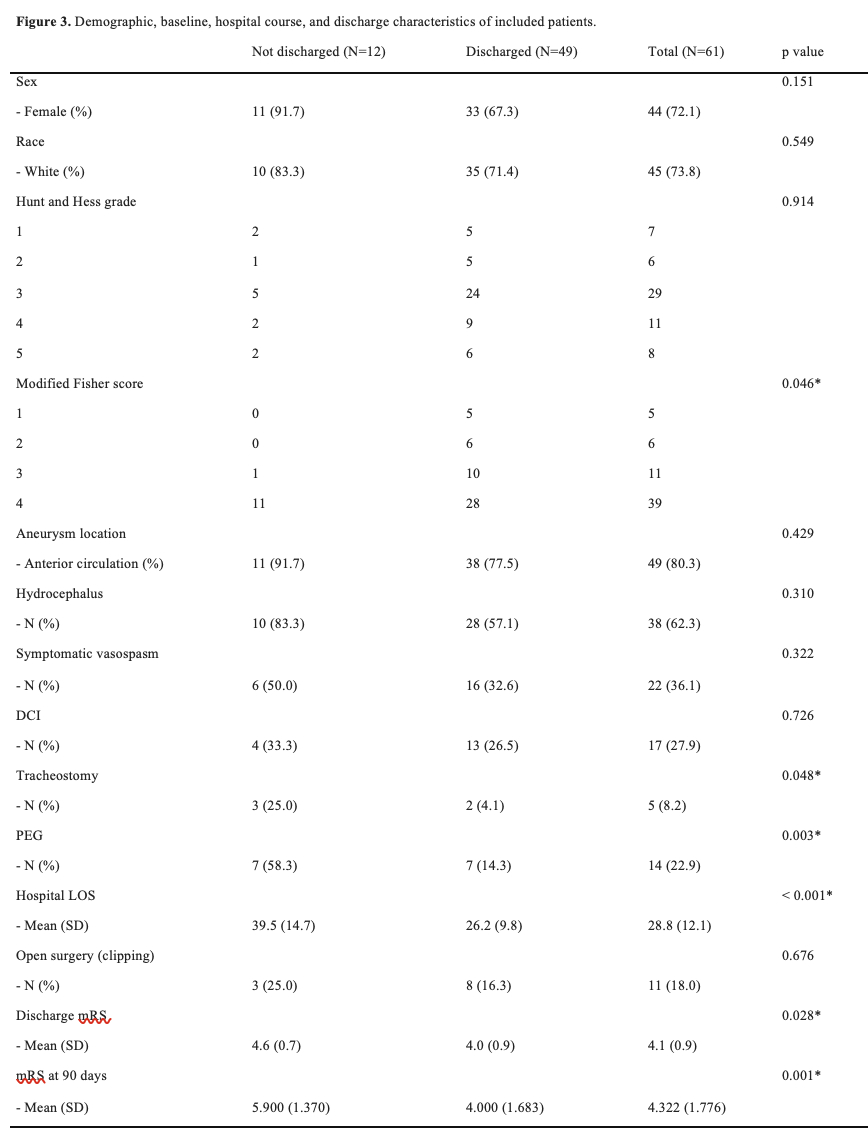
Results: Of 450 aSAH patients, 61 (13.5%) were discharged to a SNF. No patients discharged to LTAC returned home and were not reviewed further. Among SNF patients, 49 (80.3%) were discharged home (Figure 1). Discharged patients were younger (mean 63.3±11.5 years vs. 70.2±9.3, p=0.040; Figure 2) and had lower modified Fisher scores (3 [IQR 3-4] vs. 4 [IQR 4-4], p=0.046; Figure 3). Intraventricular hemorrhage (OR 0, 95% CI 0-1.12, p=0.043), tracheostomy (OR=0.14, 95% CI 0.14-1.01, p=0.048), and gastrostomy tube (PEG) placement (OR=0.13, 95% CI 0.03-0.51, p=0.003) were associated with lower odds of SNF discharge. Patients discharged home had shorter hospital LOS (26±10 vs. 39±15 days, p<0.001) and lower mRS scores at discharge (4 [IQR 4-5] vs. 5 [IQR 4-5], p=0.028) and 90-days post-discharge (4 [IQR 3-5] vs. 6 [IQR 5-6], p=0.001). Multivariable regression identified old age, PEG and hospital LOS as independent predictors of SNF discharge. Tracheostomy, PEG, and symptomatic vasospasm predicted SNF LOS.
Conclusions: A majority of aSAH patients were discharged from SNF to home. Those not discharged were more medically complex with neurological deficits. These results may guide goals of care discussions, suggesting that patients unfit for home discharge may benefit from SNF placement to bridge hospitalization and independence.
More abstracts on this topic:
Oikonomou Evangelos, Holste Gregory, Coppi Andreas, Baloescu Cristiana, Mcnamara Robert, Khera Rohan
Assessing Short-Term Prognostic Value of eGFR Formulas in Patient with Acute Heart Failure: Comparison of Chronic Kidney Disease Epidemiology Collaboration 2021, 2009 Formula, and Modification of Diet in Renal Disease in Asian Population – A Study from VietnamTran Dieu Hien, Do Chau, Nguyen Thi Kim Chuc, Pham Ngoc Anh Vu, Phan Hoang Son, Phan Tri Cuong, Han Nguyen Le My, Nguyen Thi Huong Dung, Vo Le Y Nhi, Cao Doan Thi Bich Huyen, Tran Thanh Phong, Truyen Thien Tan Tri Tai, Tran Van Duong, Nguyen Ngoc Huyen, Pham Thanh Phong, Nguyen Minh Nghiem, Nguyen Van Khoa, Vo Phuc Dai, Le Hoang Phuc, Dinh Quang Minh Trí, Vu Loc, Kieu Doan Thi
Readers' Comments
We encourage you to enter the discussion by posting your comments and questions below.
Presenters will be notified of your post so that they can respond as appropriate.
This discussion platform is provided to foster engagement, and simulate conversation and knowledge sharing.
You have to be authorized to post a comment. Please, Login or Signup.