Final ID: DP11
Association Between Pre-Stroke Cardiovascular Risk with Post-Stroke Cognitive Decline and Dementia: A Pooled Analysis of Four Cohort Studies
Methods: We included 1,808 dementia-free individuals with incident stroke (91% ischemic, 7% hemorrhagic, 2% other; 52% women, 38% Black, median age 75) from 4 cohorts (1971-2019): Atherosclerosis Risk In Communities Study, Cardiovascular Health Study, Framingham Offspring Study, and REasons for Geographic And Racial Differences in Stroke. We assessed prestroke atherosclerotic cardiovascular disease (ASCVD) risk with the American Heart Association’s Predicting Risk of cardiovascular disease EVENTs (PREVENT) 10-year ASCVD risk score, which has age and sex as risk factors. Outcomes were global cognition (primary), executive function, memory, and dementia. Linear mixed-effects and Cox regression models examined continuous and categorical (quintiles) 10-year ASCVD risk scores and adjusted for mean prestroke cognition, race, education, and cohort. Median (IQR) follow-up was 4.4 (2.0, 7.9) years for global cognition and 5.1 (2.4, 8.8) for dementia. Dementia cases totaled 142 at 5 years and 182 at 10 years.
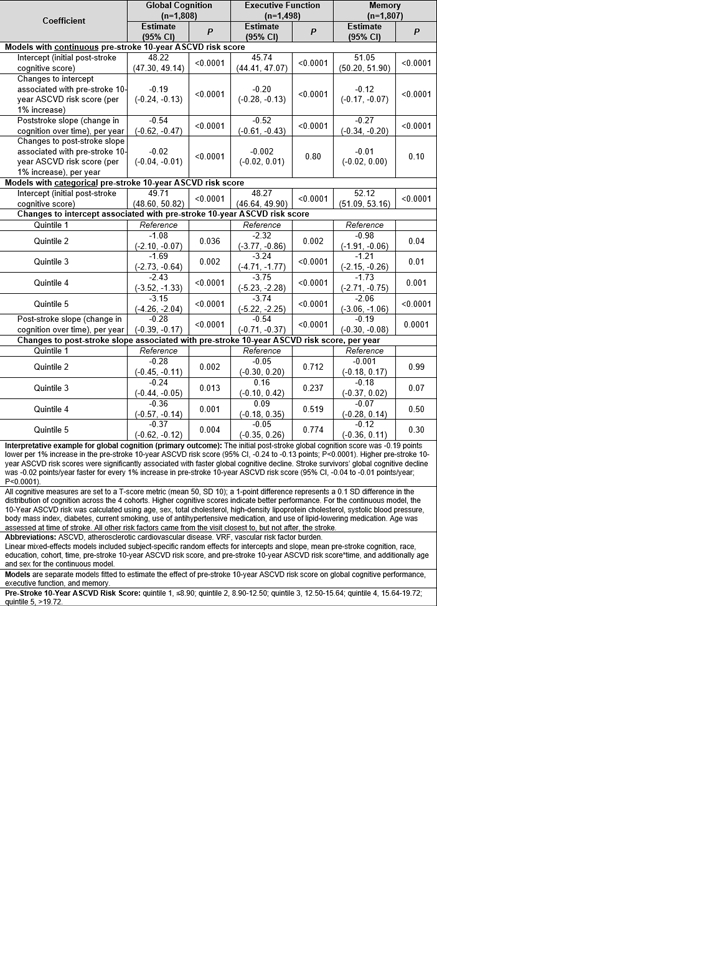
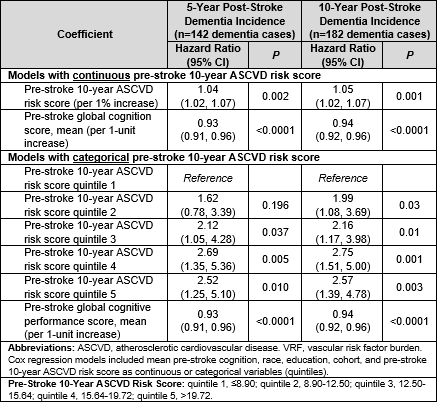
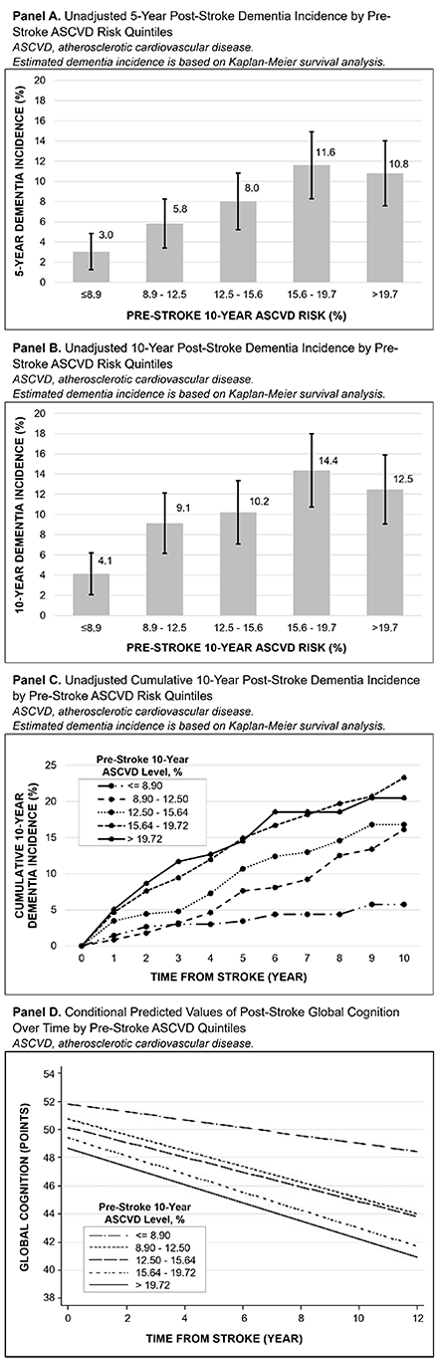
Results: Median (IQR) 10-year prestroke ASCVD risk was 14.0% (9.9%, 18.5%). Higher prestroke 10-year ASCVD risk was associated with lower adjusted initial poststroke global cognition, memory, and executive function (changes to intercept, Table 1). The quintile analysis showed a dose-response relationship between higher prestroke ASCVD risk and lower initial poststroke cognition scores (changes to intercept, Table 1). The overall stroke survivor group had unadjusted mean declines of -0.59 points/year (95%CI, -0.66 to -0.52 points/year; P<0.001) for global cognition, -0.54 points/year (95%CI, -0.62 to -0.46 points/year; P<0.001) for executive function, and -0.35 points/year (95%CI, -0.42 to -0.28 points/year; P<0.001) for memory. Higher prestroke 10-year ASCVD risk was associated with faster global cognitive decline (P<0.001) and nominally faster memory decline (P=0.10) but not executive function decline (P=0.80) (changes to poststroke slope, Table 1). Higher quintiles of prestroke ASCVD risk were associated with faster global cognitive decline and higher 5- and 10-year dementia risk (Tables 1-2; Figure 1).
Conclusions: Higher prestroke cardiovascular risk is associated with lower initial poststroke cognitive scores, faster cognitive decline, and higher dementia risk in stroke survivors.
- Levine, Deborah ( UNIVERSITY OF MICHIGAN , Ann Arbor , Michigan , United States )
- Howard, Virginia ( UNIVERSITY OF ALABAMA-BIRMINGH , Birmingham , Alabama , United States )
- Aparicio, Hugo ( Boston University , Boston , Massachusetts , United States )
- Beiser, Alexa ( Boston University , Boston , Massachusetts , United States )
- Elkind, Mitchell ( Columbia University , New York , New York , United States )
- Gottesman, Rebecca ( NINDS , Bethesda , Maryland , United States )
- Pendlebury, Sarah ( Oxford University Hospitals NHS Tru , Oxford , United Kingdom )
- Kollipara, Adam ( Northville Public Schools , Northville , Michigan , United States )
- Cushman, Mary ( UNIVERSITY VERMONT , Colchester , Vermont , United States )
- Fohner, Alison ( University of Washington SPH , Seattle , Washington , United States )
- Koton, Silvia ( Johns Hopkins University , Baltimore , Maryland , United States )
- Hsu, Wan-ling ( University of Michigan , Ann Arbor , Michigan , United States )
- Longstreth, W ( Harborview Medical Center , Seattle , Washington , United States )
- Lopez, Oscar ( Presbyterian University Hospittal , Pittsburgh , Pennsylvania , United States )
- Seshadri, Sudha ( UT Health San Antonio , San Antonio , Texas , United States )
- Springer, Mellanie ( University of Michigan , Ann Arbor , Michigan , United States )
- Hayward, Rodney ( University of Michigan , Ann Arbor , Michigan , United States )
- Ye, Wen ( University of Michigan , Ann Arbor , Michigan , United States )
- Whitney, Rachael ( University of Michigan , Whitmore Lake , Michigan , United States )
- Sussman, Jeremy ( University of Michigan , Ann Arbor , Michigan , United States )
- Briceno, Emily ( University of Michigan , Ann Arbor , Michigan , United States )
- Gross, Alden ( Johns Hopkins University , Baltimore , Maryland , United States )
- Giordani, Bruno ( Mary A. Rackham Institute , Ann Arbor , Minnesota , United States )
- Lazar, Ronald ( Univ of Alabama at Birmingham , Birmingham , Alabama , United States )
Meeting Info:
Session Info:
Brain Health Moderated Digital Posters
Wednesday, 02/05/2025 , 01:20PM - 01:50PM
Moderated Digital Poster Abstract Session
More abstracts on this topic:
Saadat Moh, Titus Ryan, Verkuilen Haley, Fleming Phil, Sur Sanjib, Sen Souvik
3-HKA Promotes the Vascular Remodeling after Stroke by Modulating the Activation of A1/A2 Reactive AstrocytesChen Jun-min, Shi Guang, Yu Lulu, Shan Wei, Zhang Xiangjian, Wang Qun
More abstracts from these authors:
Springer Mellanie, Gottesman Rebecca, Hayward Rodney, Howard Virginia, Koton Silvia, Lazar Ronald, Sussman Jeremy, Ye Wen, Levine Deborah, Chen Bingxin, Whitney Rachael, Briceno Emily, Gross Alden, Aparicio Hugo, Beiser Alexa, Burke James, Giordani Bruno
The Association of Change in Circulating Biomarkers of Brain Injury with Cognitive Change and MRI Findings in the Cardiovascular Health StudyHayes Cellas, Djousse Luc, Lopez Oscar, Odden Michelle, Tracy Russell, Longstreth W, Fohner Alison, Bis Joshua, Psaty Bruce, Mukamal Kenneth, Seshadri Sudha, Satizabal Claudia
Readers' Comments
We encourage you to enter the discussion by posting your comments and questions below.
Presenters will be notified of your post so that they can respond as appropriate.
This discussion platform is provided to foster engagement, and simulate conversation and knowledge sharing.
You have to be authorized to post a comment. Please, Login or Signup.