Final ID: WP313
Associations of Extreme Precipitation and Cerebrovascular Disease Mortality Events Among Older Adults in California
Introduction:
In mid- to high-latitude regions, cerebrovascular diseases (CBVD) are known to peak during the winter. Aside from traditional clinical risk factors, emerging research has documented the associations between extreme seasonal climate conditions and CBVD, especially among older male and females who are vulnerable to such environments. Despite the growing climate-cerebrovascular literature, there is still a need to understand seasonal- and sex-specific associations between extreme precipitation and CBVD events among older adults. We hypothesize that extreme precipitation will increase the risk of cerebrovascular events in winter and summer for both older and male and females.
Methods:
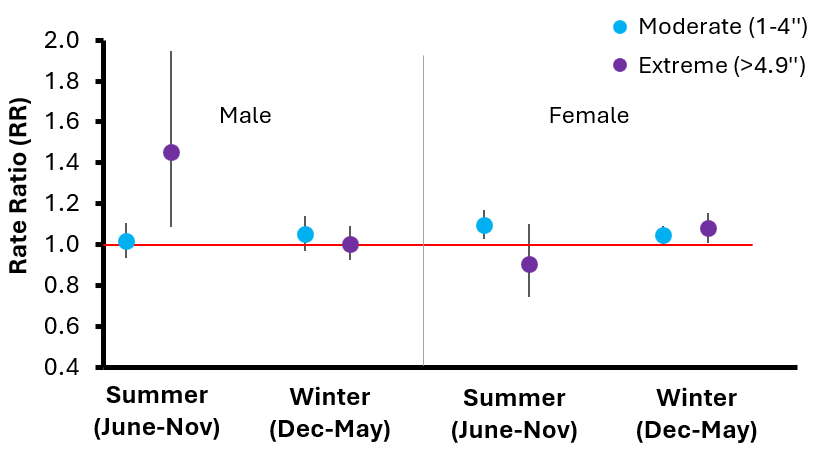
This population-based study utilizes CDC county data for CBVD deaths [ICD-10 (I60-69)] among older (≥65 years) male and females in California (N=28 counties) from January 2016 to December 2020. Covariates of diabetes, smoking, obesity, excessive drinking, uninsured prevalence, household income, and college education attainment were also obtained. Precipitation was classified as; extreme (>90th percentile: >4.9 inches), moderate (10-90th percentile: 1-4 inches), and low (≤10th percentile: ≤1 inch). With population estimates, CBVD mortality rates were associated with precipitation categories by sex and season [winter (December-May) and summer (June-November)] using negative binomial regression with autocorrelation upon adjusting for covariates. Model estimated parameters were interpreted as a rate ratio (RR).
Results:
From 2016-2020; 59,360 (61.8% females; 52.6% in winter) CBVD deaths were recorded. Extreme (compared to low) precipitation was associated with increased risk of CBVD mortality rates for males only during the summer [adjusted RR 1.45 (95% CI 1.08-1.95)], not winter (Figure). Whereas extreme precipitation was associated with increased risk of CBVD mortality rates for females only during the winter [1.08 (95% CI 1.01-1.15)]. Significant interactions were observed between precipitation and maximum temperatures.
Conclusion:
Extreme precipitation was associated with increased risk of CBVD deaths among older males and females, where the effects differed by season. Seasonality and climate factors can be considered predisposing risk factors for cerebrovascular disease. Further studies are needed to assess such risks for other areas in the United States.
More abstracts on this topic:
Correa Fabiano Ronaldo, Bittencourt Marcio, Bosco Mendes Thiago, Romero-nunez Carlos, Generoso Giuliano, Staniak Henrique, Foppa Murilo, Santos Raul, Lotufo Paulo, Bensenor Isabela
Adverse Pregnancy Outcomes and Offspring Cardiovascular Health in Early AdulthoodLam Emily, Notterman Daniel, Lloyd-jones Donald, Allen Norrina, Shah Nilay, Gauen Abigail, Khan Sadiya, Freedman Alexa, Stein James, Venkatesh Kartik, Tawa Elisabeth, Savas Hacer, Goldman Noreen
Readers' Comments
We encourage you to enter the discussion by posting your comments and questions below.
Presenters will be notified of your post so that they can respond as appropriate.
This discussion platform is provided to foster engagement, and simulate conversation and knowledge sharing.
You have to be authorized to post a comment. Please, Login or Signup.