Final ID: FR446
FLUDROCORTISONE VS MIDODRINE FOR ORTHOSTATIC HYPOTENSION: A RETROSPECTIVE COHORT STUDY
Abstract Body: Introduction:
Orthostatic hypotension (OH) is a debilitating condition commonly observed in patients with impaired vascular tone upon positional changes, often due to neurogenic disorders, liver disease, hypovolemia, or advanced HF. While fludrocortisone has been associated with adverse outcomes—particularly HF-related complications—compared to midodrine in HF populations, direct comparative data between these two therapies in the general population with OH is seldom.
Hypothesis:
This study aims to compare cardiovascular and renal outcomes in patients with OH treated with fludrocortisone (without midodrine) versus those treated with midodrine (without fludrocortisone).
Methods:
A retrospective cohort study was conducted using data from the TriNetX collaborative research network from January 2007 to May 2025. Patients aged 18 or older diagnosed with OH were included. After propensity score matching for demographics, comorbidities, and medications, two cohorts were analyzed: cohort 1 included 33,101 patients treated with fludrocortisone (excluding midodrine), and cohort 2 included 33,101 treated with midodrine (excluding fludrocortisone). Mean age was 62 years; 51% were female and 47% male. Risk ratios (RR) and hazard ratios (HR) with 95% confidence intervals and p-values were calculated using TriNetX. The outcomes assessed included all cause mortality, syncope/collapse, stroke, heart failure (HF), acute myocardial infarction (AMI), atrial fibrillation (AF), and ventricualr fibrillation (VF).
Results:
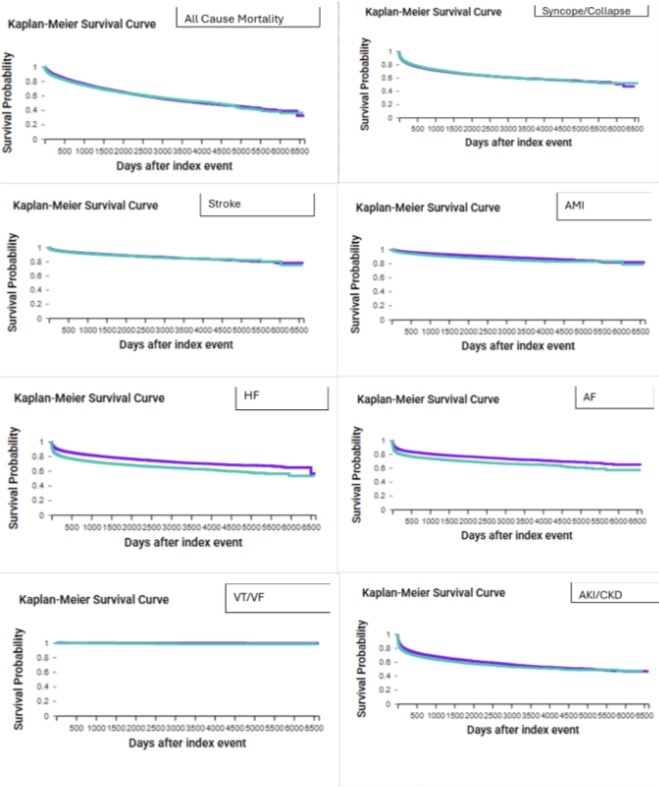
Though mortality risk was higher in cohort 1 (26.85% vs. 22.12%, RR 1.214, 95% CI 1.181–1.247; p<0.0001), HR was 0.938 (95% CI 0.91–0.968; p<0.0001). Syncope was more frequent in cohort 1 (25.84% vs. 21.77%, RR 1.187; p<0.0001; HR 1.034; p=0.025), as was stroke (8.09% vs. 7.09%, RR 1.142; HR 0.939; p=0.0375). AMI (6.05% vs. 6.92%, RR 0.873; HR 0.694; p<0.0001), HF (17.81% vs. 22.99%, RR 0.775; HR 0.636; p<0.0001), AF (18.50% vs. 22.54%, RR 0.821; HR 0.695; p<0.0001), and VF (0.34% vs. 0.62%, RR 0.544; HR 0.435) were all lower in cohort 1. AKI/CKD risk was similar (30.43% vs. 30.66%, RR 0.993; p=0.5213), though HR favored fludrocortisone (0.846; p<0.0001).
Conclusion:
In OH patients, midodrine was linked to lower all-cause mortality risk, but fludrocortisone showed better survival and lower risks of HF, AMI, AF, VF, and cardiovascular mortality. Syncope and cerebrovascular events were more common with fludrocortisone.
Orthostatic hypotension (OH) is a debilitating condition commonly observed in patients with impaired vascular tone upon positional changes, often due to neurogenic disorders, liver disease, hypovolemia, or advanced HF. While fludrocortisone has been associated with adverse outcomes—particularly HF-related complications—compared to midodrine in HF populations, direct comparative data between these two therapies in the general population with OH is seldom.
Hypothesis:
This study aims to compare cardiovascular and renal outcomes in patients with OH treated with fludrocortisone (without midodrine) versus those treated with midodrine (without fludrocortisone).
Methods:
A retrospective cohort study was conducted using data from the TriNetX collaborative research network from January 2007 to May 2025. Patients aged 18 or older diagnosed with OH were included. After propensity score matching for demographics, comorbidities, and medications, two cohorts were analyzed: cohort 1 included 33,101 patients treated with fludrocortisone (excluding midodrine), and cohort 2 included 33,101 treated with midodrine (excluding fludrocortisone). Mean age was 62 years; 51% were female and 47% male. Risk ratios (RR) and hazard ratios (HR) with 95% confidence intervals and p-values were calculated using TriNetX. The outcomes assessed included all cause mortality, syncope/collapse, stroke, heart failure (HF), acute myocardial infarction (AMI), atrial fibrillation (AF), and ventricualr fibrillation (VF).
Results:
Though mortality risk was higher in cohort 1 (26.85% vs. 22.12%, RR 1.214, 95% CI 1.181–1.247; p<0.0001), HR was 0.938 (95% CI 0.91–0.968; p<0.0001). Syncope was more frequent in cohort 1 (25.84% vs. 21.77%, RR 1.187; p<0.0001; HR 1.034; p=0.025), as was stroke (8.09% vs. 7.09%, RR 1.142; HR 0.939; p=0.0375). AMI (6.05% vs. 6.92%, RR 0.873; HR 0.694; p<0.0001), HF (17.81% vs. 22.99%, RR 0.775; HR 0.636; p<0.0001), AF (18.50% vs. 22.54%, RR 0.821; HR 0.695; p<0.0001), and VF (0.34% vs. 0.62%, RR 0.544; HR 0.435) were all lower in cohort 1. AKI/CKD risk was similar (30.43% vs. 30.66%, RR 0.993; p=0.5213), though HR favored fludrocortisone (0.846; p<0.0001).
Conclusion:
In OH patients, midodrine was linked to lower all-cause mortality risk, but fludrocortisone showed better survival and lower risks of HF, AMI, AF, VF, and cardiovascular mortality. Syncope and cerebrovascular events were more common with fludrocortisone.
More abstracts on this topic:
A First-In-Human Phase 1 Study of the Safety, Tolerability, and Pharmacodynamics of REGN7544, a Novel Natriuretic Peptide Receptor 1–Blocking Monoclonal Antibody
Ahmed Mohsin, Morton Lori, Olenchock Benjamin, Herman Gary, Wynne Chris, Marin Ethan, Tuckwell Katie, Xu Meng, Cheng Xiping, Redington Emily, Koyani Bharatkumar, Mateo Katrina, Thakur Mazhar, Devalaraja-narashimha Kishor
12,13-diHOME Attenuates Pro-Arrhythmic Effect of High-Fat DietBuck Benjamin, Baer Lisa, Deschenes Isabelle, Chinthalapudi Krishna, Gallego-perez Daniel, Stanford Kristin, Hund Thomas, Areiza Natalia, Xu Xianyao, Elliott Austin, Wan Xiaoping, Nassal Drew, Lane Cemantha, Nirengi Shinsuke, James Natasha Maria