Hypertension 2025 Scientific Sessions
/
Poster Session 2 with Breakfast Reception
/
Population-wide blood pressure reduction and estimated hypertension incidence, cardiovascular disease events, and healthcare costs in Black adults: A simulation using Jackson Heart Study data
Final ID: FR521
Population-wide blood pressure reduction and estimated hypertension incidence, cardiovascular disease events, and healthcare costs in Black adults: A simulation using Jackson Heart Study data
Abstract Body: Background. Black adults in the U.S. have higher rates of hypertension compared to White adults, contributing to disparities in cardiovascular disease (CVD). Quantifying the health and economic impact of population-wide systolic blood pressure (SBP) reductions may inform the development of cost-effective nonpharmacologic strategies to prevent hypertension and CVD.
Methods. We used the CVD Policy Model, a validated simulation of blood pressure (BP) management and CVD risk, to estimate 10-year health and economic outcomes associated with population-wide, sustained SBP reductions of 2 to 10 mmHg among Black adults without hypertension. For comparison, we estimated BP, CVD, and economic outcomes associated with observed BP trajectories in a cohort derived from Jackson Heart Study participants without hypertension, defined as SBP <130 mmHg, diastolic BP <80 mmHg, no antihypertensive medication use, and no self-reported hypertension. Outcomes included incident hypertension, CVD events, quality-adjusted life years (QALYs; cost-effectiveness threshold of $100,000/QALY), healthcare costs, and cost-effectiveness of nonpharmacologic interventions. National estimates were scaled using National Health and Nutrition Examination Survey and U.S. Census data.
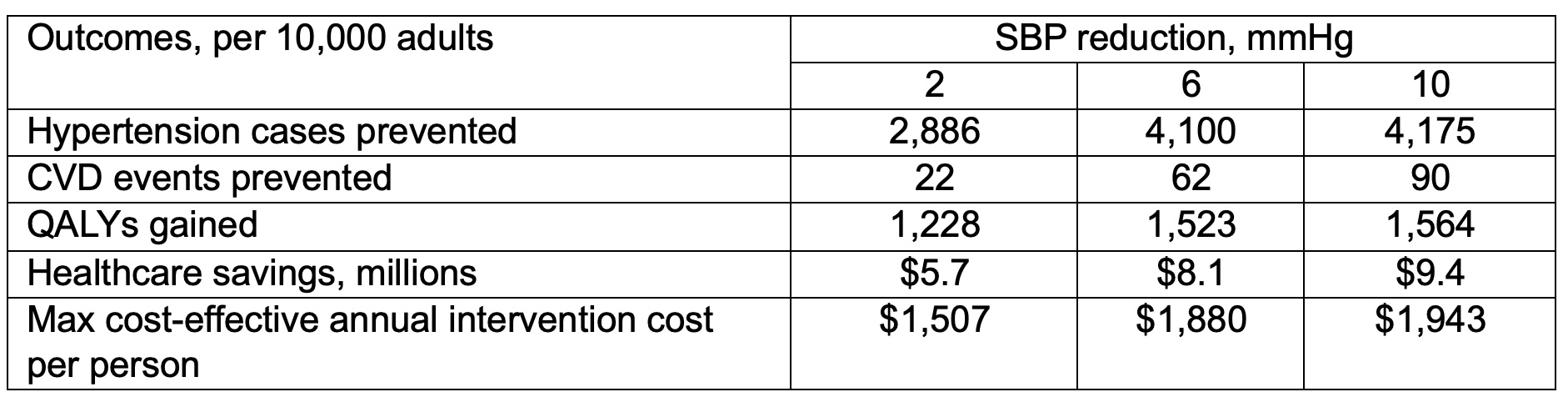
Results. Among 10,000 Black adults (mean age 47 years) without hypertension, the observed BP trajectories projected that 4,624 adults would develop hypertension, and 416 CVD events would occur over 10 years. Sustained SBP reductions of 2 to 10 mmHg were projected to prevent 62% to 90% of hypertension cases and avert 5% to 22% of CVD events over 10 years (Table). For example, a sustained 6-mmHg SBP reduction was projected to prevent 88% of hypertension cases (4,100 cases) and avert 15% of CVD events (62 events) over 10 years. A 6-mmHg SBP reduction would save $8.1 million in healthcare costs and would be cost-effective if costing ≤$1,880 per person per year. Extrapolated to the 11.5 million Black adults without hypertension in the US, a 6-mmHg SBP reduction could prevent 292,988 hypertension cases and 3,385 CVD events annually, saving $589 million in healthcare costs.
Conclusion. Sustained, population-wide SBP reductions of 2 to 10 mmHg in Black adults without hypertension could reduce hypertension incidence, CVD events, and healthcare spending and are potentially cost-effective.
Methods. We used the CVD Policy Model, a validated simulation of blood pressure (BP) management and CVD risk, to estimate 10-year health and economic outcomes associated with population-wide, sustained SBP reductions of 2 to 10 mmHg among Black adults without hypertension. For comparison, we estimated BP, CVD, and economic outcomes associated with observed BP trajectories in a cohort derived from Jackson Heart Study participants without hypertension, defined as SBP <130 mmHg, diastolic BP <80 mmHg, no antihypertensive medication use, and no self-reported hypertension. Outcomes included incident hypertension, CVD events, quality-adjusted life years (QALYs; cost-effectiveness threshold of $100,000/QALY), healthcare costs, and cost-effectiveness of nonpharmacologic interventions. National estimates were scaled using National Health and Nutrition Examination Survey and U.S. Census data.
Results. Among 10,000 Black adults (mean age 47 years) without hypertension, the observed BP trajectories projected that 4,624 adults would develop hypertension, and 416 CVD events would occur over 10 years. Sustained SBP reductions of 2 to 10 mmHg were projected to prevent 62% to 90% of hypertension cases and avert 5% to 22% of CVD events over 10 years (Table). For example, a sustained 6-mmHg SBP reduction was projected to prevent 88% of hypertension cases (4,100 cases) and avert 15% of CVD events (62 events) over 10 years. A 6-mmHg SBP reduction would save $8.1 million in healthcare costs and would be cost-effective if costing ≤$1,880 per person per year. Extrapolated to the 11.5 million Black adults without hypertension in the US, a 6-mmHg SBP reduction could prevent 292,988 hypertension cases and 3,385 CVD events annually, saving $589 million in healthcare costs.
Conclusion. Sustained, population-wide SBP reductions of 2 to 10 mmHg in Black adults without hypertension could reduce hypertension incidence, CVD events, and healthcare spending and are potentially cost-effective.
- Hardy, Shakia ( Univ of North Carolina Chapel Hill , Mebane , North Carolina , United States )
- Moran, Andrew ( Columbia University Medical Center , New York , New York , United States )
- Ogedegbe, Olugbenga ( NYU LANGONE HEALTH , New York , New York , United States )
- Spruill, Tanya ( NYU SCHOOL OF MEDICINE , New York , New York , United States )
- Ravenell, Joseph ( NYU LANGONE MEDICAL CENTER , New York , New York , United States )
- Safford, Monika ( WEILL CORNELL MEDICINE , New York , New York , United States )
- Shimbo, Daichi ( COLUMBIA UNIVERSITY , New York , New York , United States )
- Muntner, Paul ( University of Alabama at Birmingham , Birmiham , Alabama , United States )
- Bellows, Brandon ( Columbia University , New York , New York , United States )
- Foti, Kathryn ( University of Alabama at Birmingham , Birmiham , Alabama , United States )
- Zhang, Yiyi ( COLUMBIA UNIVERSITY , New York , New York , United States )
- Carson, April ( Univ of Mississippi Medical Center , Jackson , Mississippi , United States )
- Cherrington, Andrea ( University of Alabama at Birmingham , Birmingham , Alabama , United States )
- Commodore-mensah, Yvonne ( JOHNS HOPKINS SCHOOL OF NURSIN , Baltimore , Maryland , United States )
- Cooper, Lisa ( JOHN HOPKINS UNIV SCH OF MEDICINE , Baltimore , Maryland , United States )
- Juraschek, Stephen ( BIDMC-Harvard Medical School , Boston , Massachusetts , United States )
- Levy, Phil ( Wayne State , Detroit , Michigan , United States )
Author Disclosures:
Shakia Hardy: DO NOT have relevant financial relationships
| Andrew Moran: No Answer
| Olugbenga Ogedegbe: No Answer
| Tanya Spruill: No Answer
| Joseph Ravenell: No Answer
| Monika Safford: No Answer
| Daichi Shimbo: DO NOT have relevant financial relationships
| Paul Muntner: No Answer
| Brandon Bellows: DO NOT have relevant financial relationships
| Kathryn Foti: DO NOT have relevant financial relationships
| Yiyi Zhang: DO have relevant financial relationships
;
Research Funding (PI or named investigator):NIH/NHLBI:Active (exists now)
| April Carson: DO NOT have relevant financial relationships
| Andrea Cherrington: No Answer
| Yvonne Commodore-Mensah: No Answer
| Lisa Cooper: No Answer
| Stephen Juraschek: DO NOT have relevant financial relationships
| Phil Levy: No Answer
Meeting Info:
Session Info:
More abstracts on this topic:
A multifaceted family intervention for blood pressure management in rural China: an open label, parallel group, cluster randomized trial (Healthy Family Program)
Jiang Chao, Dong Jianzeng, Cai Jun, Anderson Craig, Du Xin, Tang Yangyang, Han Rong, Song Yanna, Wang Chi, Lin Xiaolei, Yi Yang, Rodgers Anthony, Ma Changsheng
A Nationwide Italian Network for the Clinical and Genetic Diagnosis of Familial Dyslipidemias: The LIPIGEN registryCasula Manuela, Galimberti Federica, Olmastroni Elena, Arca Marcello, Averna Maurizio, Catapano Alberico
More abstracts from these authors:
Discuss the measurement, incorporation, and analysis of social determinants of health in lifestyle interventions
Breathett Khadijah, Carson April, Hardy Shakia
Role of Hypertension in the Cardiovascular-Kidney-Metabolic Syndrome among Black Adults: The Jackson Heart StudyDubal Medha, Colantonio Lisandro, Arabadjian Milla, Tanner Rikki, Muntner Paul, Ghazi Lama, Bertoni Alain, Carson April, Lewis Cora, Alanaeme Chibuike, Johnson Dayna, Shimbo Daichi, Foti Kathryn
You have to be authorized to contact abstract author. Please, Login
Not Available