Final ID: TH252
Impact of a Curriculum on Outpatient Management of Hypertensive Urgencies at a VA Primary Care Clinic
Abstract Body: Background
Hypertensive urgency (HU) is defined as a systolic blood pressure (SBP) ≥ 180 mm Hg and/or diastolic blood pressure (DBP) ≥ 110 mm Hg without evidence of end-organ damage. Guidelines recommend aggressive antihypertensive medication uptitration for patients presenting with HU in the outpatient setting. An HU curriculum delivered to Yale internal medicine (IM) residents in February-March 2023 was shown to improve residents’ confidence and knowledge in HU and was also associated with greater improvement in treatment intensification among residents who did versus did not receive the curriculum at a Federally Qualified Health Center in New Haven, CT. Here we report the curriculum’s effects on residents’ outpatient HU management at the West Haven VA Medical Center (WHVA).
Methods
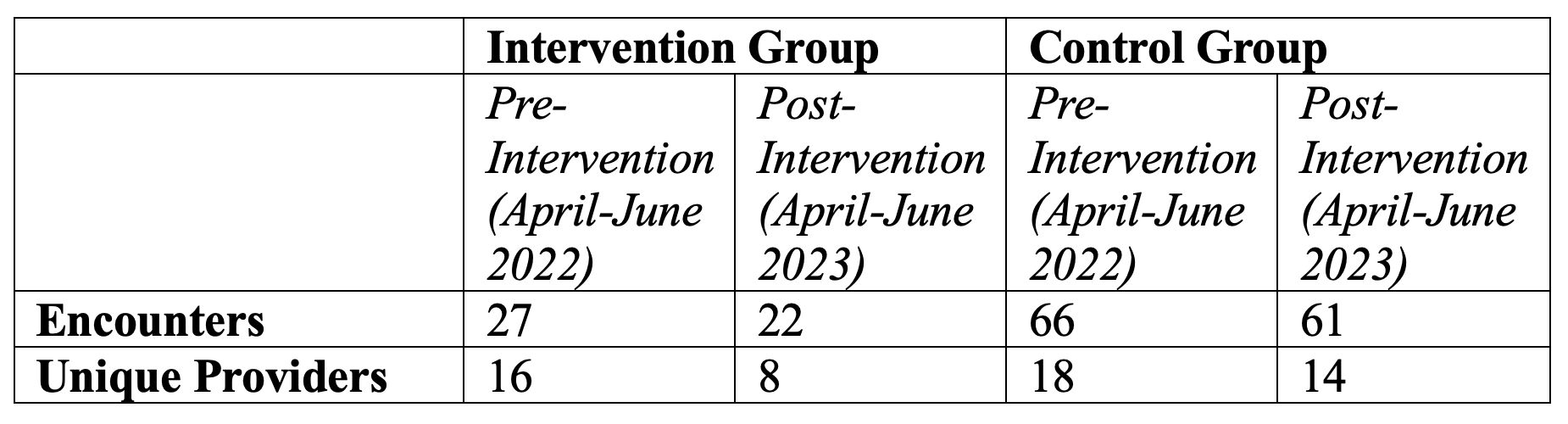
In the primary care clinic at the WHVA, patients are seen by IM residents (intervention group), who received the curriculum, and attending physicians and APRNs (control group), who did not. We included all encounters with BP in the HU range in April-June 2022 (pre-intervention period) and April-June 2023 (post-intervention period). In this preliminary analysis, one adjudicator reviewed providers’ notes to determine the change in total hypertension daily dose (HDD), a validated measure of antihypertensive treatment intensity. We performed a difference-in-differences (DID) analysis using linear regression to model the change in HDD with time and group effects; the beta coefficient for the interaction term between time and group is equivalent to the DID effect.
Results
There were 176 eligible encounters (Table). The mean (SD) SBP and DBP were 190 (11) mm Hg and 88 (13) mm Hg, respectively. In the intervention group, the mean (SD) change in HDD was 0.52 (0.79) post-intervention vs. 0.20 (0.47) pre-intervention (difference 0.32). In the control group, the mean (SD) change in HDD was 0.25 (0.52) post-intervention vs. 0.36 (0.59) pre-intervention (difference -0.12). There was greater post- vs. pre-intervention improvement in change in HDD in the intervention group vs. control group (DID 0.44 [95% CI 0.05 – 0.82]).
Conclusion
At a VA primary care clinic, an HU curriculum was associated with greater improvement in antihypertensive treatment intensification among IM residents (who received the curriculum) compared to attendings and APRNs (who did not). However, treatment intensification was inadequate in both groups, and further work is needed to improve guideline adherence in the clinic.
Hypertensive urgency (HU) is defined as a systolic blood pressure (SBP) ≥ 180 mm Hg and/or diastolic blood pressure (DBP) ≥ 110 mm Hg without evidence of end-organ damage. Guidelines recommend aggressive antihypertensive medication uptitration for patients presenting with HU in the outpatient setting. An HU curriculum delivered to Yale internal medicine (IM) residents in February-March 2023 was shown to improve residents’ confidence and knowledge in HU and was also associated with greater improvement in treatment intensification among residents who did versus did not receive the curriculum at a Federally Qualified Health Center in New Haven, CT. Here we report the curriculum’s effects on residents’ outpatient HU management at the West Haven VA Medical Center (WHVA).
Methods
In the primary care clinic at the WHVA, patients are seen by IM residents (intervention group), who received the curriculum, and attending physicians and APRNs (control group), who did not. We included all encounters with BP in the HU range in April-June 2022 (pre-intervention period) and April-June 2023 (post-intervention period). In this preliminary analysis, one adjudicator reviewed providers’ notes to determine the change in total hypertension daily dose (HDD), a validated measure of antihypertensive treatment intensity. We performed a difference-in-differences (DID) analysis using linear regression to model the change in HDD with time and group effects; the beta coefficient for the interaction term between time and group is equivalent to the DID effect.
Results
There were 176 eligible encounters (Table). The mean (SD) SBP and DBP were 190 (11) mm Hg and 88 (13) mm Hg, respectively. In the intervention group, the mean (SD) change in HDD was 0.52 (0.79) post-intervention vs. 0.20 (0.47) pre-intervention (difference 0.32). In the control group, the mean (SD) change in HDD was 0.25 (0.52) post-intervention vs. 0.36 (0.59) pre-intervention (difference -0.12). There was greater post- vs. pre-intervention improvement in change in HDD in the intervention group vs. control group (DID 0.44 [95% CI 0.05 – 0.82]).
Conclusion
At a VA primary care clinic, an HU curriculum was associated with greater improvement in antihypertensive treatment intensification among IM residents (who received the curriculum) compared to attendings and APRNs (who did not). However, treatment intensification was inadequate in both groups, and further work is needed to improve guideline adherence in the clinic.
More abstracts on this topic:
The inadequacy of Physician’s Knowledge of Iron Deficiency Anemia in Heart Failure
Bess Olva, Tung George, Toral Lama Alejandro
A Multimodality Education Model Improves Healthcare Professionals' Competency in Managing Cardiovascular Risk Factors in Type 2 Diabetes: A Mixed-Methods StudyMadhusudhan Divya, Pressley Alyssa, El Sayed Nuha, Okeke Oge, Bradley Sarah, Blanco Caroline, Perla Esteban, Jennings Ruby, Picou Kylie, Mcweeny Patrick, Crabill Carrianne