Final ID: 42
Fecal Microbiota Transplantation Decreases Autoantibody Production and Lowers Blood Pressure in an Experimental Model of Autoimmune Disease
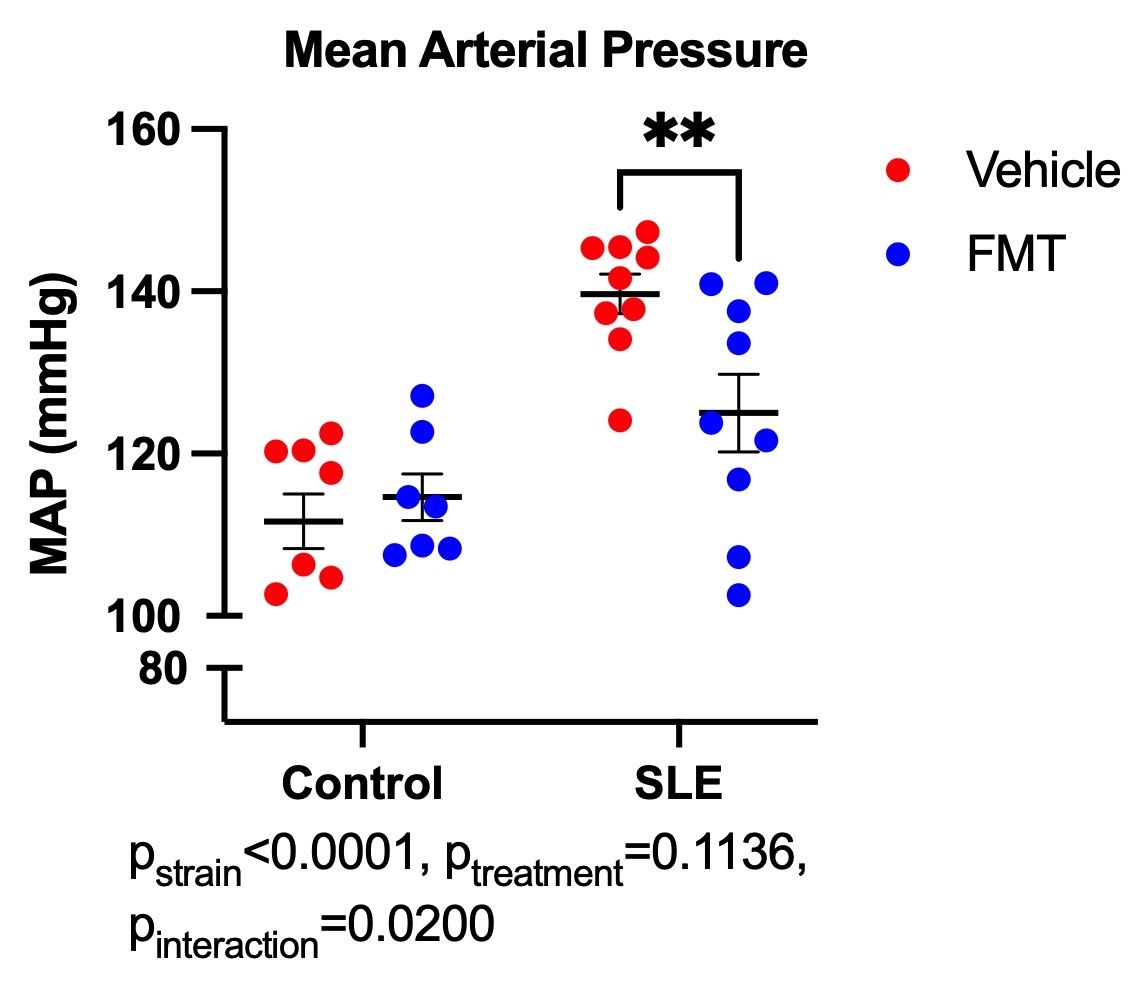
Abstract Body: Systemic lupus erythematosus (SLE) is a chronic multisystem autoimmune disorder that disproportionately affects women. It is characterized by a breach of immunological self-tolerance and the expansion of autoreactive T and B lymphocytes, leading to the production of autoantibodies. Autoantibody production leads to downstream chronic inflammation resulting in high rates of hypertension, renal injury, and cardiovascular disease. Gut dysbiosis is associated with many autoimmune diseases, including SLE. In the present study, we hypothesized that gut dysbiosis in SLE may play a role in the development of immune system dysfunction and hypertension in an experimental model of SLE, and that fecal microbiota transplantation (FMT) with microbes from control mice may improve these parameters. To test this hypothesis, we treated 26-week-old female control (NZW, n=10) and SLE (NZBWF1, n=9) mice with broad spectrum antibiotics in drinking water for one week to deplete the existing microbiota. Subsequently, mice were given 0.1 mL of fecal microbes from either control or SLE mice via oral gavage two times per week for four weeks in the following groups (n=9-10 mice/group): Control-vehicle, Control-SLE microbes, SLE-vehicle, SLE-Control microbes. Changes in the gut microbiome after FMT were assessed by metagenomic sequencing of fecal pellets from all four groups. Mean arterial pressure (MAP, mmHg) was higher in SLE mice compared to control mice (Control: 112±3 vs. SLE: 140±2 mmHg, p<0.0001). SLE mice that received FMT with control microbes had lower blood pressure (SLE-FMT: 126±4 mmHg, p=0.03). While there were no changes in circulating and splenic B cell percentages, SLE mice had significantly higher percentages of CD11b+CD11c+ autoimmune-associated B cells compared to control mice (Control: 0.41±0.04% vs. SLE: 1.2±0.1%, p=0.0006), which were significantly decreased in SLE-FMT mice (SLE-FMT: 0.76±0.1%, p=0.02). Circulating autoantibodies were also measured at the conclusion of the study. Anti-dsDNA IgG was elevated in SLE mice compared to control (Control: 149±38 vs. SLE: 527±114 kU/mL, p=0.02), and were significantly lower in SLE mice treated with control microbes (SLE-Control microbes: 126±4 mmHg, p=0.03). These data suggest that gut microbiota present in NZBWF1 mice contribute to the accumulation of activated B cells and increased autoantibody production, which are known pathogenic factors in the development of hypertension in SLE.
More abstracts on this topic:
Associations of Fiber-Rich Dietary Patterns with the Gut Microbiome: Finding from the Baltimore Longitudinal Study of Aging
Chen Yingan, Tanaka Toshiko, Tilves Curtis, Chia Chee, Mueller Noel
2 Dimensional Echocardiography versus 3 Dimentional Echocardiography to Assess Right Ventricular Function in Pulmonary Hypertension: A Systematic ReviewChaudhry Waleed Razzaq, Hajj Fatima, Bathula Satyamedha, Meghji Mohammed Askari, Pasupuleti Hemalatha, Kiyani Madiha, Shah Syeda Simrah, Neelakantan Ramaswamy Sanathanan, Mirzaeidizaji Nakisa, St. Jacques Jahnoy, Khan Khalil Ullah, Veluchamy Elakkiya, Jesse Joshanna